****
ISCHEMIA: MASKED STEMI
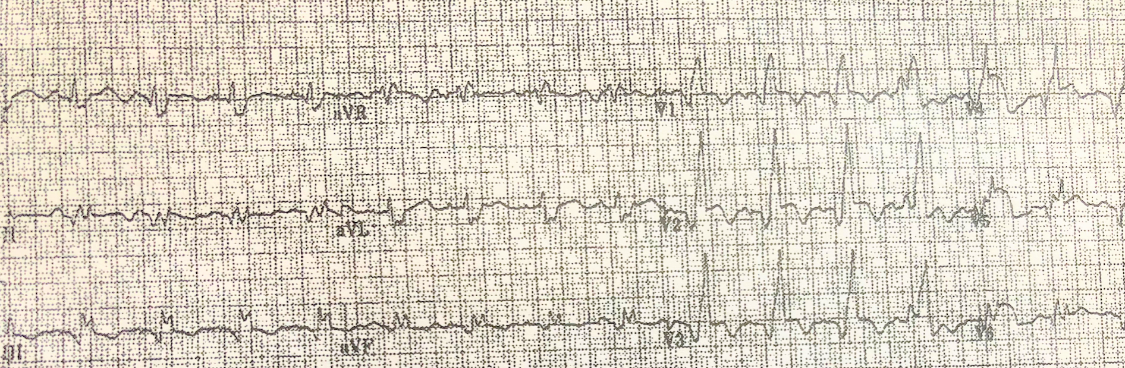
MI & RBBB:
- “The presence of RBBB may confound the diagnosis of STEMI” – 2017 ESC guidelines European Society of Cardiology
- In RBBB the ST segments are normally isoelectric except for slight ST depression V1-V3.
- If any ST elevation, worry
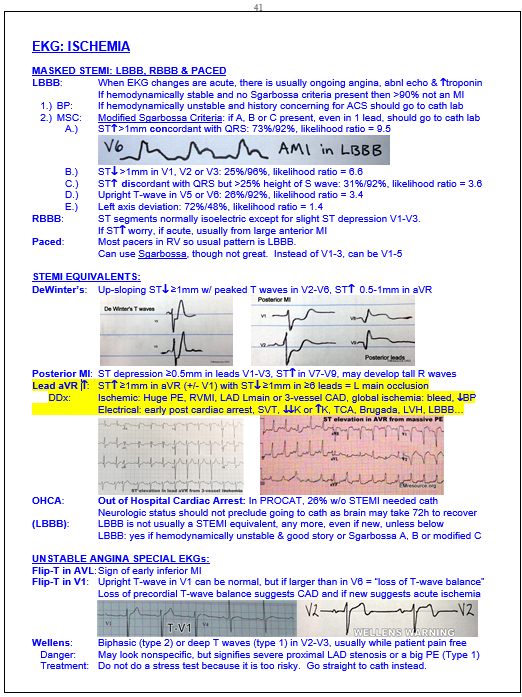
MI & LBBB: Smith-modified Sgarbossa Criteria:
- Any one criteria in LBBB or paced rhythm suggests AMI,
- If no criteria then >90% not an MI
- With AMI there is usually ongoing angina, abnl echo & troponin rise
- Criteria with sensitivity%/specificity%
- Discordant ST elevation >25% of S-wave: 31%/92%
- ST elevation >1 mm that is inappropriately concordant:73%/92%
- ST depression >1 mm in V1, V2 or V3: 25%/96%
- Upright T-wave in V5 or V6: 26%/92%.
- Left axis deviation: 72%/48%
MI & Pacer:
- Most pacers in RV so normal pattern is a LBBB.
- If LBBB pattern then use either original or Smith-modified Sgarbossa:
- Less accurate except #1: ST elevation >5mm or 25% S-wave: 53%/88%
****
ISCHEMIA: STEMI EQUIVALENTS
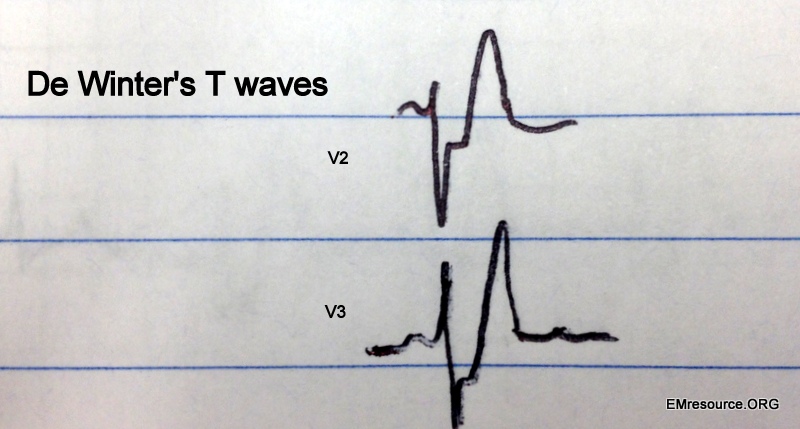
De Winter’s T-waves:
- Precordial leads: V1-V5
- Upsloping ST depression >1 mm
- Tall/peaked T waves
- Associated with proximal LAD occlusion
- Great article on T-wave inversion: click here
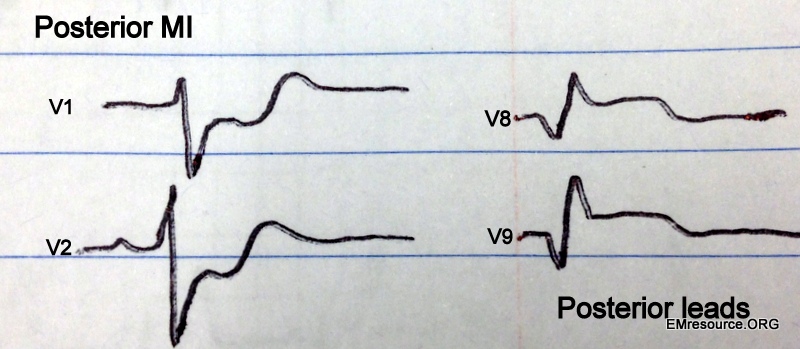
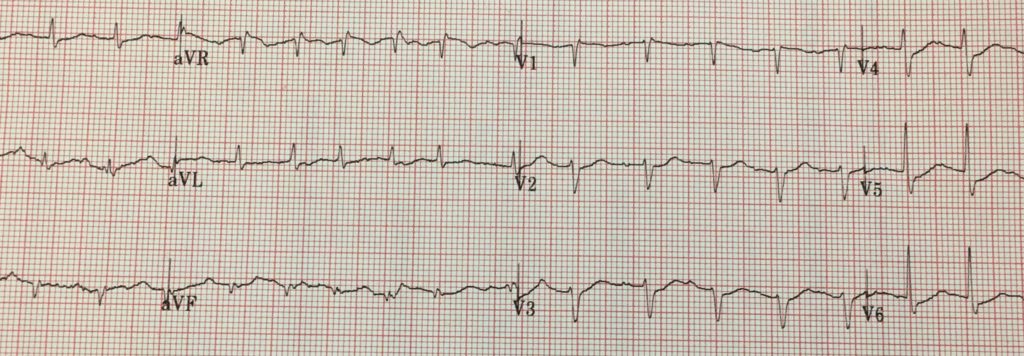
Posterior MI:
- ST depression >0.5 mm in leads V1-V3 with upright T waves
- May develop tall R waves in V1-V3
- ST elevation in posterior leads: V7- V9,
Out of Hospital Cardiac Arrest:
- In PROCAT, 96% w/ & 26% w/o STEMI needed PCI
- Neurologic status should not preclude going to cath
- brain may take 72 hours to recover
Lead AVR & Left Main Occlusion:
- ST elevation >1 mm in aVR and often V1 also
- ST depression >1 mm in 6 or more leads
- ST elevation in AVR can be from RVMI, left main or triple vessel disease
- DDx: massive PE or Brugada syndrome, (for more see page shot above)
No Longer necessarily a STEMI equivalent:
- Left Bundle Branch Block is rarely a STEMI equivalent:
- only if hemodynamically unstable & good story, even if new
- Consult cardiology for EKG findings below
- Consider thrombolytics or cath lab activation
****
ISCHEMIA: EKG SPECIAL CASES
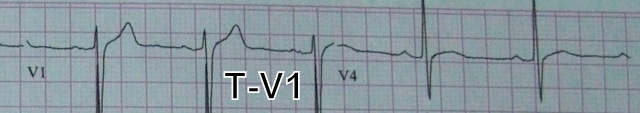
T-V1:
- A large upright T-wave in V1 can be suggestive of acute ischemia,
- This is especially true if it is new or larger than the T-wave in V6 (loss of T-wave balance)
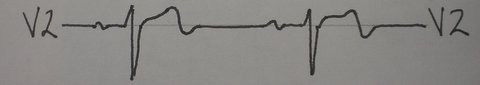
Wellens:
- Biphasic or deep T waves in V2-V3 (DDx = PE) usually while patient pain free
- May look nonspecific, but signify severe proximal LAD stenosis
- Do not do a stress test because it is too risky. Go straight to cath instead.
Old EKG:
- If EKG shows unchanged ST or T wave abnormalities it may still mean ischemia
- Should know under what clinical circumstances old EKG was done.
- It may have been w/ ACS and therefore not the patient’s baseline
****
See page-shot below from my Tarascon book that summarizes info above
****
SYNCOPE: ESSENTIAL EKGs
Brugada Syndrome:
EKG: Downsloped or saddleback ST in V1-V3 often w/ T-inversion &/or RBBB
3 types shown below. Findings can be intermittent
DDx: K, Ca, drug toxicity, RV injury/infarct, normal variant (no syncope)
Treatment: AICD (drugs don’t work). 10%/year die w/o AICD. Screen family as 50% familial
Hypertrophic CardioMyopathy:
Symptoms: Syncope oft w/ exertion +/- M, usual age of dx 30-40
EKG: Q-waves in I & avL, v5-v6 or II & III that are deep and narrow. (Biphasic T, LVH)
Long QT:
Risks for torsades: Slow HR, CHF/MI, dehydrated, female, Talternans. Trigger: startle/pain
Diagnosis: 99th percentile for normal: QTc >470 in men & QTc >480 in women. QTc >500: danger
Meds: (see qtdrugs.org or A to Z Pharmacopoeia), CAD, ¯K/¯Mg/¯Ca/¯PO4
Congenital: Romano-Ward (can hear) & Jaervell-Lang-Nielson (deaf)
Lown-Ganong-Levine:
What: Basically it’s WPW (see below) without the delta wave
EKG: Short PR in all leads, no delta wave in any lead.
Rx: Same as WPW (see below)
RV Dysplasia:
What: Big RA and RV is electrically silent as is all scar/fat. Get V-tach.
EKG: V1-V3 inverted T, fragmented QRS, Epsilon wave (notch at end of QRS), (low voltage).
Wolff-Parkinson-White:
What: Pre-excitation due to conduction tract bypassing the AV node
EKG: Persistant short PR in all leads, delta wave in any one lead, episodic SVT or a-fib…
DDx: No delta wave: Lown-Ganong-Levine, low Ca, ASD, junctional, (nl variant if PR >105ms)
****
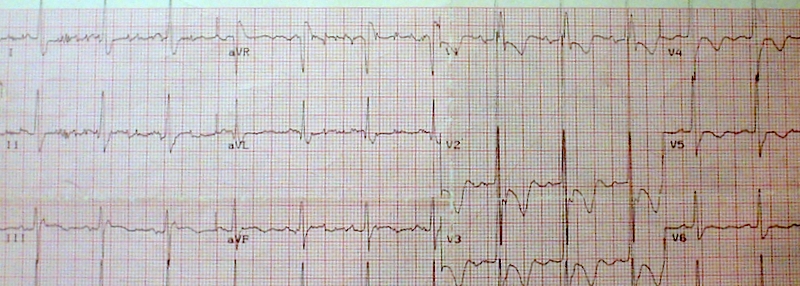
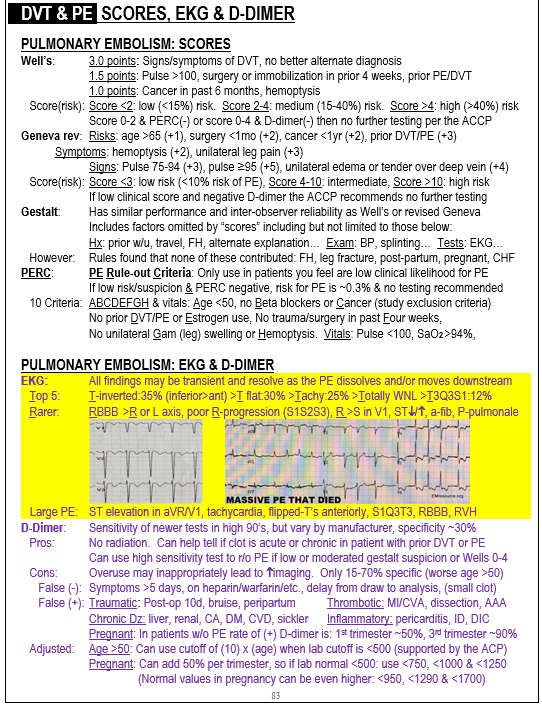
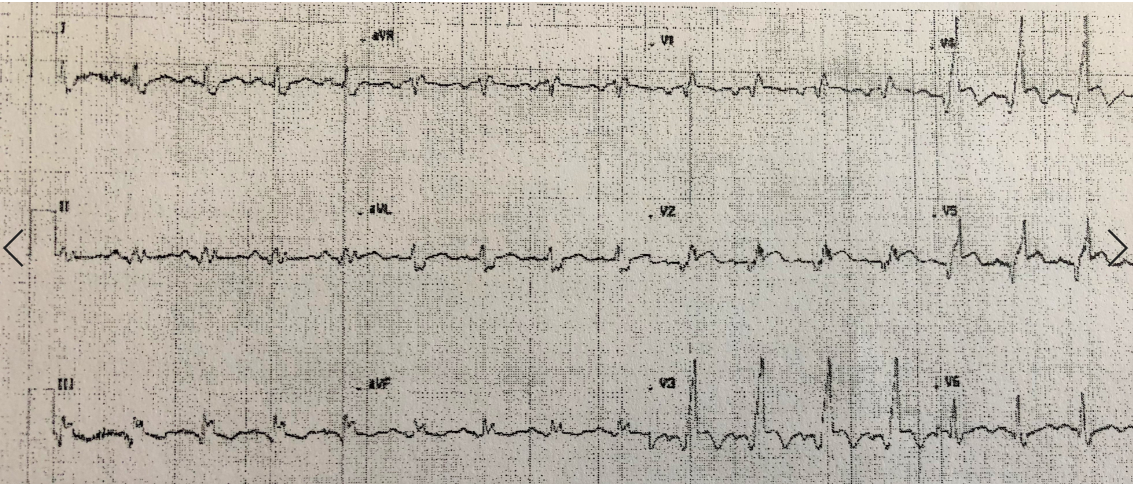
PE EKG’s
Beware: “Classic” is Latin for 15% of the time. This is especially true of PE’s, where many cases present atypically.
- Isolated small PE’s present with pleuritic chest pain and normal vitals. There may be no other signs or symptoms and EKG is usually completely normal without tachycardia. Send a D-dimer if you have no better explanation for the pain. 20% have no known risk factors
- Isolated large PE’s are often painless and the only symptoms are SOB or DOE. EKG changes can mimic ACS, CXR can mimic pneumonia, and WBC can be elevated.
Below are some EKG findings you may or may not have heard of. Remember the EKG is usually only abnormal in LARGE PE’s
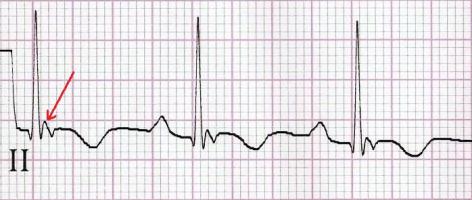
***Anterior T inversion***
Great article on T-wave inversion: click here
*** Sinus tachycardia with nonspecific T and ST changes***