Vital Sign Pearls from Episode 20 of EM Logic Podcast
A lot of the med-mal cases I review involve missed vital sign red flags. The main ones include the following: unexplained tachycardia, soft BP, minor temperature elevation <100.4, and mild hypoxia. Not all patients with one or more of these vital sign red flags is going to get into trouble if they are sent home, but some of them are. Let’s dig deeper
- Heart Rate: We were all taught the normal HR for an adult is 60-100, but logic and experience tells me that things are much more complicated than that. For a healthy patient a normal heart rate is more like 50-90 and really varies depending on the physiologic and emotional state. If the heart rate is in the 90’s or even high 80’s, pay attention, especially if the BP is on the soft side. They may be in compensated shock. Only 25% of PE’s have a HR >100 but about 40% have HR >90. SIRS criteria used HR >90
- Temperature: Few ER patients without infection have a temperature >98.6. A lot of people are usually closer to 97.6 than 98.6. If the temperature is 98.8 or higher pay attention. It may mean nothing or something depending on the clinical presentation. Also, they say with each 1 degree Fahrenheit the heart rate goes up about 10 bpm, but I don’t think one causes the other because I frequently notice the HR rise before the temperature.
- Blood Pressure: if the diastolic BP is <50 think about sepsis and early pressors if it doesn’t come up with fluids. Literature says every hour delay increased mortality.
- Shock Index: Compare the HR and SBP. Normally HR/SBP should be <0.7 (eg. BP 100 and HR 70 is potentially borderline) If the HR is approaching the SBP pay attention. It may signify compensated shock. If the HR is equal to or greater than the SBP (eg. HR 98, BP 96/55) you should really worry
- Bilateral BP: Not useful for diagnosing aortic dissection (difference >20mmHg in 40% of dissections and 20% of normals). Critical for treating BP in aortic dissection or other hypertensive emergencies as well as hypotensive emergencies. Which arm do you use? It’s a trick question. Always use the higher arm, as this is usually the true BP.
- Respirations and Pulse-ox: Tachypnea can be due to anxiety but can also be from sepsis, PE, metabolic acidosis and a number of other conditions. Also remember that oxygen is more likely to do harm than good in a patient who doesn’t need it. Oxygen can cause vasoconstriction, can cause lung damage, and can lead to CO2 narcosis in susceptible individuals. In general, titrate to O2sat of 92-96%, except for COPD use 89-94%
- Pediatric Vital Signs. Fortunately most EMR’s will now flag abnormal vital signs for age. Nevertheless you should have a resource you check or formula you use, especially for the heart rate. I use 165 -s 10(age) and the following webpage: https://em1minuteconsult.com/?page_id=2124
Physical Exam Pearls from Episode 6 of EM Logic Podcast
- Head-Jolt sign: This is about 99% sensitive and 50% specific for meningitis. Have patients rapidly turn their head side to side. If it doesn’t hurt or they have to do it twice, make sure they don’t have meningitis. I will often grab their head and do it for them, but first definitely explain what I am doing to family members.
- Eyes-Red eyes: Consensual photophobia or limbal flush suggests iritis or keratitis rather than conjunctivitis.
- Pulmonary exam: Demonstrating how you want them to breathe and having them breathe more rapidly in and out is quicker and more sensitive for abnormal lung sounds. If you think you hear consolation when performing lung exam, ask a yes or no question. This can help continue your history, speed up your exam, and identify a pneumonia (a sort of modified egophony). After that and the end of an exhale, tell them to stop breathing and stick out their tongue (if no mask) while you listen to the heart with your stethoscope closer to the heart and without interference from lung sounds or, worse yet, speech. Bonus: Look at their tongue for hydration status.
- Vascular-Pulses in the feet: Comparing pedal pulses is critical when there is a possibility of a knee dislocation, an aortic dissection, or acute limb ischemia, all of which can be sneaky and time-sensitive. Popliteal arterial injuries often are diagnosed late due to severe leg pain or spontaneous knee reduction. Aortic dissection rarely extends into an arm but almost always extends into a leg. Acute limb ischemia can mimic DVT, sciatica, or even a stroke.
- Ortho-Pain location: Have them touch the exact spot that hurts the most. Without this and a confirmatory exam, you may end up imaging the wrong part of the spine or extremity. If you are lucky, it will only cause a delay; if you are not, it can cause a disaster. I have seen many misses or near misses due to this.
- Ortho-Arm/hand neuro exam: Have the patient make an OK sign with the wrist in dorsiflexion and third fourth and fifth fingers spread apart. This allows you to evaluate the median (C5-8), ulnar (C8-T1), and radial nerves (C6-C8) in a five-second motor exam.
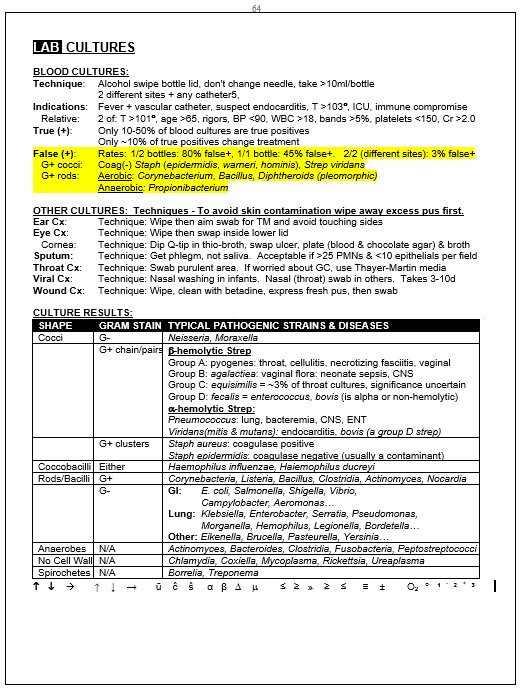
Blood cultures are usually useless and probably lead to unnecessary callbacks more often than change in management. More specifics below
test
