Even though many are named “RULES”, they should not be. Instead they should be considered TOOLS, CRITERIA, SCORES or perhaps GUIDELINES.
The goal is to decrease imaging and thereby radiation and improve ED throughput. A head to toe run of my most frequently used decision tools and scores are listed below.
IMPORTANT: you should know the exclusion criteria for each study. Some of these decision tools have additional blind spots.
Shared Decision Making: To minimize risk of patient complaints and other “complications”, when not imaging, it may be useful to discuss the small remaining risk (usually 1-2%) with patient, chance they may need to return if worse or not better, and to document shared decision making. If you want to copy our shared decision making template click here
****
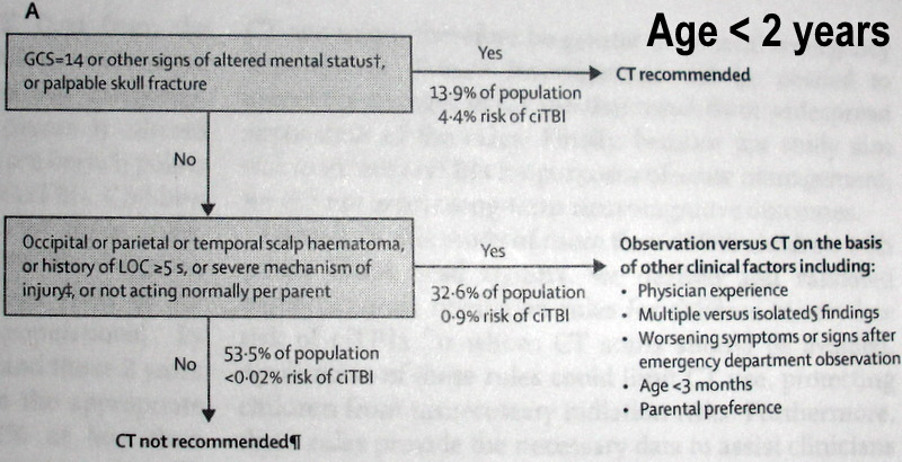
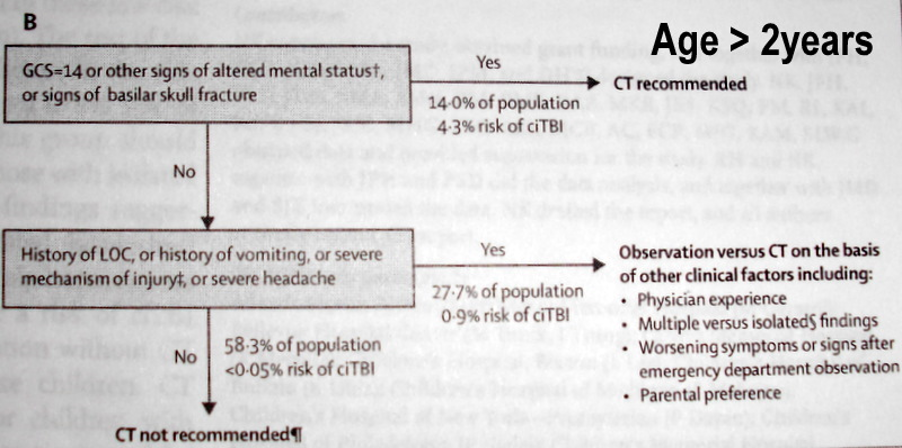
HEAD: PECARN
Included: n = 42,412, age <18, GCS =15 (~5% +CT, ~1% ciTBI and ~1/1000 need surgery)
Excluded: >24h, ground level fall, walking into object, prior CNS disease, penetrating injury
Abbreviations: ciTBI = clinically important Traumatic Brain Injury, PECARN = Pediatric Emergency Care Applied Research Network
Criteria: See charts below from the PECARN head injury study
Branch 1: AMS, abnormal neuro exam of e/o skull fracture on exam: risk of ciTBI >4% so CT all
Branch 2: Risk of ciTBI ~1% if any of below factors present: CT or close observation w/o CT
- Age <2y: risky/unknown mechanism*, LOC >5 sec, palpable fx, non-frontal hematoma, vomit
- Age >2y: risky mechanism*, any LOC, signs of basilar skull fx, vomiting, severe HA
If Branch 2 positive then decision whether or not to CT should be based on: # of factors present, worsening or not, provider experience & parent preference. Isolated LOC <1 minute, isolated nonprogressive HA or isolated vomiting entails a risk <1%. If multiple branch 2 red flags present then the risk is >1% risk so should order CT
* Risky Mechanism: Fall >5 stairs or >5ft, or if age <2y >3ft (height of sink/counter but not bed/table), Head struck by projectile or high-impact object, bad MVA, skating/scooter/bike w/o helmet
Benefit: decreases CT’s by 20-25%. Cancer risk of CT ~1/5,000.
Validated: YES
****
HEAD: NEXUS II
Included: N =13,728 with head injury
Excluded: delay to care >24 hours
Abbreviations: NEXUS = National Emergency X-radiography Utilization Study
Criteria/Mnemonic: BEAN BASH: Blood thinner, Emesis, Age >65, Neuro or Behavior abnl, AMS, Skull fx, Hematoma
Sensitivity: 98.3% for significant injury (not + CT).
Benefit: 13% for all 8 criteria plus exclusion criteria
Conclusion: Can’t construct a rule that is any better than clinical judgement
****
HEAD: CANADIAN HEAD CT RULES
Included: N = 3121.
Excluded: Age <16, delay to care >24 hours, blood thinners, seizure
5 High risk criteria: GCS<15 @ 2h, sign of skull fx, vomiting >1, age >65y
2 Additional criteria: amnesia >30m, bad mechanism
Sensitivity: 100% (92-100%) for intervention using top 5, 98% for abnormal CT using all 7
Benefit: Scans reduced by 32% if all 7 criteria, and by 54% if only the 5 high risk criteria
****
HEAD: Merit based Incentive Payment System (MIPS)
Caveats: Not a study, but a CMS policy so should be defensible
Policy: If head CT for trauma ordered, then document a reason below
Age >18: 1 of: severe HA, emesis, mechanism, thin blood, focal deficit, e/o skull fx, age >65
Age <18: If head CT ordered document: “Patient NOT low risk according to PECARN criteria”
Mnemonic: HEMATOMAS:
- Headache that is severe/worsening
- Emesis (even once)
- Mechanism (see PECARN for concerning mechanisms)
- Amnesia/KO >1 minute
- Thin blood: Plavix, etc. riskier for acute bleed but less risky for delayed bleed than blood thinners
- Observed & worse (We apply to ED obs or presentation beyond 24 hours)
- Memory: if they don’t get 3/3 at 5 minutes, 2 tries allowed
- Age >65
- AMS
- Skull fracture clinically: step-off or basilar
****
NECK: NEXUS C-SPINE RULES
Included: 834,069 patients. 818 fractures
Excluded: Age <2, direct blow or penetrating injury, severe osteoporosis, cancer, severe arthritis
Abbreviations: NEXUS = National Emergency X-radiography Utilization Study
Criteria: No intoxication, no distracting injury, A+Ox4, no neuro deficit, no midline spinal tenderness
Sensitivity: 99% sensitive for any neck fracture, 99.6% sensitive for clinically significant fracture
Caveats: Few patients age <8 in study
Benefit: If all criteria below satisfied then no imaging. # of x-rays reduced by 33%
Other: No distracting injury was not defined. The way I do it is to ask the patient something like, “when you are not moving anything do you have any pain that you feel is strong enough to distract you from noticing another injury?”
****
NECK: CANADIAN C-SPINE RULES
Included: 8924 patients. 151 fractures
Excluded: AMS, age <16, pregnant, paralysis, penetrating injury, repeat visit, prior neck disease
Exclusion: AMS/intoxication, age <16, pregnant, paralysis, penetrating injury, repeat visit.
Low Risk: Simple rear-end MVA or ambulatory or delayed onset of pain or no midline tenderness
High Risk: Age >65, paresthesia, bad mechanism: fall >3ft, axial load, bad MVA, bike/ATV, rollover…
Application: If any low risk & no high risk criteria & can rotate 45° left & right then no x-ray
Sensitivity: 100% (98-100%) sensitive for clinically significant fracture.
Benefit: # of x-rays reduced by 42% if criteria plus exclusion criteria satisfied
****
CHEST: P.E.R.C. CRITERIA
Included: 8138 patients with chief complaint of dyspnea or chest pain
Excluded: Cancer, Beta-blocker use, medium or high clinical suspicion of PE
Criteria:
- pulse <100, SaO2 >94%
- Aae <50
- no DVT or PE history
- no estrogen use
- no immobilization in past 4 weeks
- no unilateral leg swelling
- no hemoptysis
Mnemonic combining Criteria + Exclusions: Vital signs & ABCDEFGH:
- Pulse <100, SaO2 >94%
- Age <50
- no Beta blockers
- no Cancer
- no DVT or PE history
- no Estrogen use
- past Four weeks – no immobilization
- no Gam (leg) swelling that is unilateral
- no Hemoptysis
Sensitivity: 98%
Benefit: No need for D-Dimer or advanced imaging in 22%
Blind Spots: Active cancer, use of medications that lower the heart rate, medium or high clinical suspicion of PE
More info: https://pubmed.ncbi.nlm.nih.gov/18318689/
****
CHEST: YEARS CRITERIA
Included: 346 patients to determine when can use a higher D-dimer cutoff (double usual one)
Excluded:
- Age <18y
- Blood thinner use
Abbreviations: YEARS
Criteria/Mnemonic: HAD
- No Hemoptysis
- No better Alternate diagnosis
- No clinical signs of DVT
Sensitivity: ~99%
Benefit: Using a D-dimer cutoff of 1000 (twice usual cutoff) led to 14% fewer chest CT”s.
Validated: yes
Blind Spots:
More info: https://rebelem.com/the-years-study
****
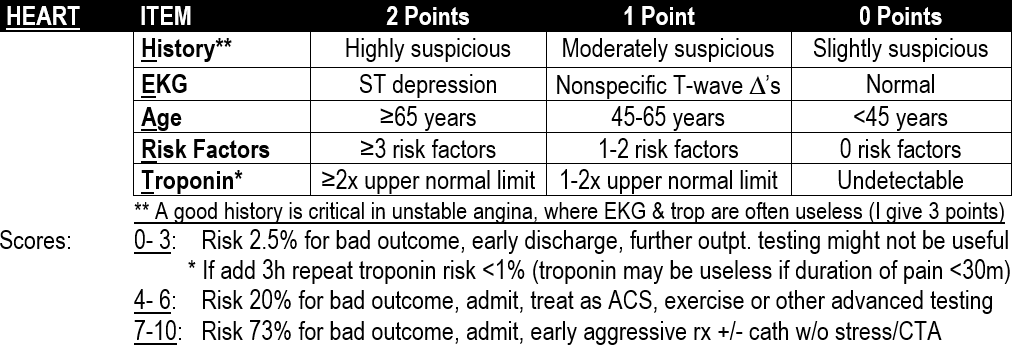
CHEST: H.E.A.R.T. SCORE
Included: N = 122 in the 2008 Netherlands derivation study: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2442661/
Excluded: No pain, STEMI (all other ED chest pain patients were included)
Criteria/Mnemonic: HEART:
Sensitivity: 97.5% but better in validation studies. (see Validated section below)
Benefit: ~20% of ED chest pain patients can be sent home. No need for admission or urgent advanced cardiac imaging if Score < 3
Blind Spots:
- If the chest pain has resolved and lasted <30 minutes then the EKG, troponin and repeat troponin may all be completely useless. In such cases I would consider doubling the points for history. If it is highly suspicious, give four points and if moderately suspicious give 2 points
- If the AVERAGE risk for all comers in the low risk group (scores of 0-3) is in the 1% range after a repeat troponin, and those with scores of 2 or 3 have a higher risk than those with scores of 0 or 1, then it follows that those with a score of 0 or 1 likely have a risk <1%, but those with a score of 2 or 3 likely have a risk >1%.
Validated: YES, by multiple studies:
- N = 303, MACE = 1% in low risk
- N = 2440. MACE = 1.7% in low risk group: https://www.ncbi.nlm.nih.gov/pubmed/23465250
- N =1070. MACE = 0% if low risk and repeat troponin at 3 h negative, but confidence interval 72-100%
- N = 1107, MACE = 1% if low risk and repeat troponin at 3 h negative
****
CHEST: Canadian Syncope Risk Score of 2016:
Included: 4030 pts, <24h since syncope, no obvious reason to admit, admitted or discharged
Excluded: LOC >5min, AMS after awake, witnessed seizure, major trauma, intoxication, language barrier, knocked out
Outcomes: 9.5% admitted, 3.6% adverse event rate (7-23% in prior studies, 0.2% were PE)
Criteria/Mnemonic: ABCD-TV: Axis, BP, Cardiac, Durations, Troponin, Vasovagal
- Prone to Vasovagal syncope
- No known prior Cardiac disease
- No SBP >180 or <90 while in ED
- Normal Troponin
- Normal QRS Axis (-30 to 110)
- QRS Duration <130ms
- QTc Duration <480ms
- No Cardiac syncope ED diagnosis
- Vasovagal ED diagnosis
Sensitivity:
- 99.6% if likely vasovagal, unlikely cardiac & none of the 9 criteria
- 99.2% if likely vasovagal, unlikely cardiac & only 1 of the 9 criteria
- 97.7% if likely vasovagal, unlikely cardiac & only 2 of the 9 criteria
Benefit: fewer admissions
Blind Spots: excluded patients, other EKG abnormalities, obvious indication for admission
Validated: Not as off 2020
****
CHEST: CURB-65L:
Included: 1,048 patients from the CURB-65 international derivation study
Excluded: none found so far
Criteria/Mnemonic:
- Confusion
- BUN >20
- RR >30
- BP <90/60
- 65 or older
- Lactate >2
Sensitivity:
Benefit: consider outpatient for score 0-1 as 30 day mortality <2%. I don’t trust this
Blind Spots: CURB-65 recommends sending home a pneumonia patient with a score of 1 due to new confusion, a RR >30, a BP <90/60 or a lactate >2; any of these would be very risky unless they resolved prior to discharge. CURB-65 also recommends admitting a patient just because they had a score of 2 due to a BUN >20 plus age >65 even if they otherwise look good; this also does not make clinical sense. Together these properties make the score fairly useless according to some experts.
Validated: YES, by multiple studies
****
ABDOMEN: ALVARADO SCORE
Does anyone use this for appendicitis?
****
KNEE: OTTAWA KNEE RULES
Excluded: Age <18, injury >7 days old, neuro deficit, distracting injury, paraplegia
Criteria: No X-ray if all of: age<55, patella & fibular head nontender, Can flex 90°, can walk
****
ANKLE/FOOT: OTTAWA ANKLE/FOOT RULES
Excluded: Age <18, injury >10 days old, neuro deficit, intoxication or distracting injury
Criteria: No X-ray needed if malleoli, 5th metatarsal & navicular all non-tender and can walk 4 steps
****

1. Wells, Geneva, Clinical gestalt2. Yes. If D-dimer navetige and clinical suspicion high, I image.3. Only patients who are crashing & I suspect saddle embolus AND CV surgeon not available for emergent Trendelenburg procedure.4. I admit all PE’s.