History of Present Illness: A man in his mid 70’s with a history of PVD but no known CAD presents with 2 hours of non-radiating slightly pleuritic chest pain and SOB that is exertional in nature.
Vital Signs & Physical Exam: Vital signs are normal. Physical exam is normal with clear lungs, no splinting and no murmur. Pulses are symmetric x 4 without delay
An ECG is done: focus on these 8 leads
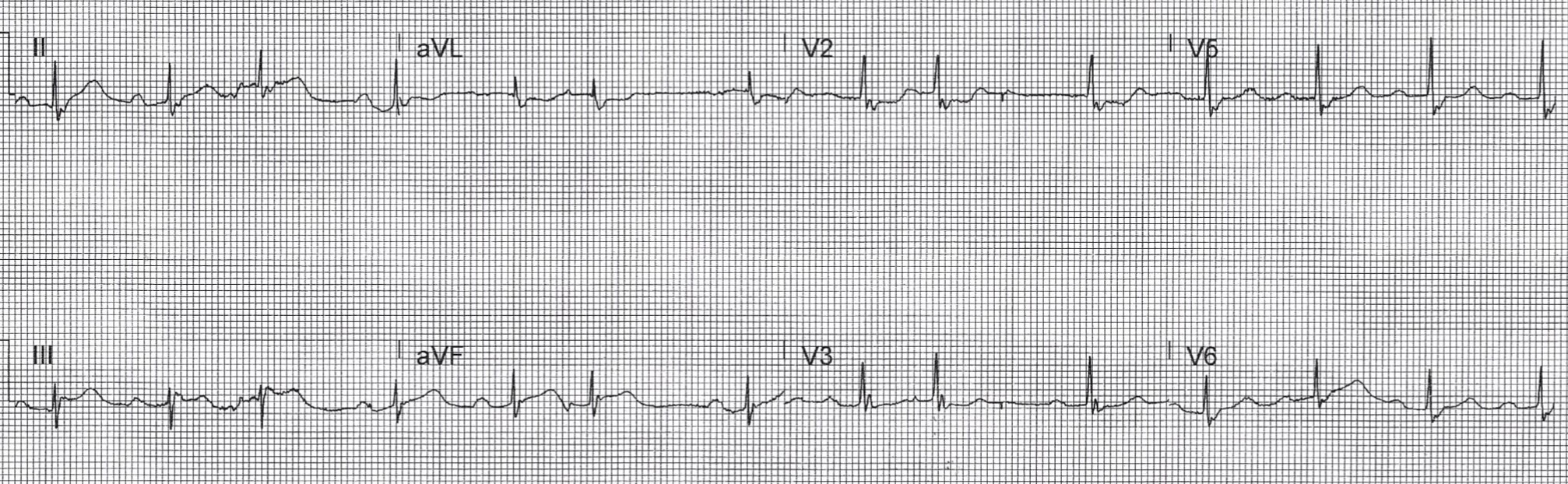
Computer Read: NSR at 80, first degree AV block, PAC’s, RBBB
What is the most likely cause of ECG findings in this patient?
- A) STEMI
- B) Pulmonary embolism
- C) RBBB with expected secondary ST and T wave changes
- D) OMI
SCROLL DOWN FOR ANSWERS & 1-MINUTE CONSULT
<<<<<<<<<<<<<<<<<<<<< ADVERTISEMENT & SPACER >>>>>>>>>>>>>>>>>>>>>
THE EMERGENCY MEDICINE POCKETBOOK TRIFECTA
- Emergency Medicine 1-Minute Consult, 5th edition
- A-to-Z EM Pharmacopoeia & Antibiotic Guide, 5th edition
- 8-in-1 Emergency Department Quick Reference, 5th edition
******************************************************************************
<<<<<<<<<<<<<<<<<<<<<<<<< END SPACER >>>>>>>>>>>>>>>>>>>>>>>>>
ANSWER:
- A) STEMI
- B) Pulmonary embolism
- C) RBBB with expected secondary ST and T wave changes
- D) OMI – CORRECT – There are hyperacute T waves in II and aVF with subtle ST elevation that does not meet STEMI criteria but is diagnostic of Occlusion MI.
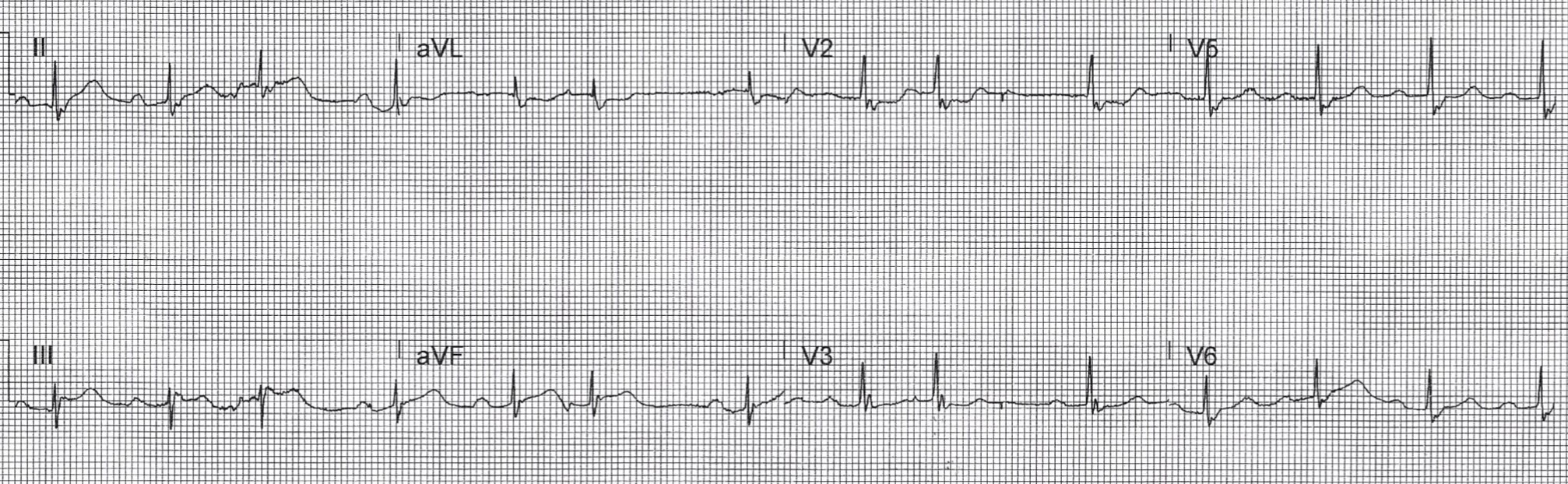
Serial ECGs:

- Computer Read: SB at 54 first degree AV block, RBBB
- My Read: reperfusion biphasic T-waves in the inferior leads and ST depression in V2/V3 back to normal levels for a RBBB
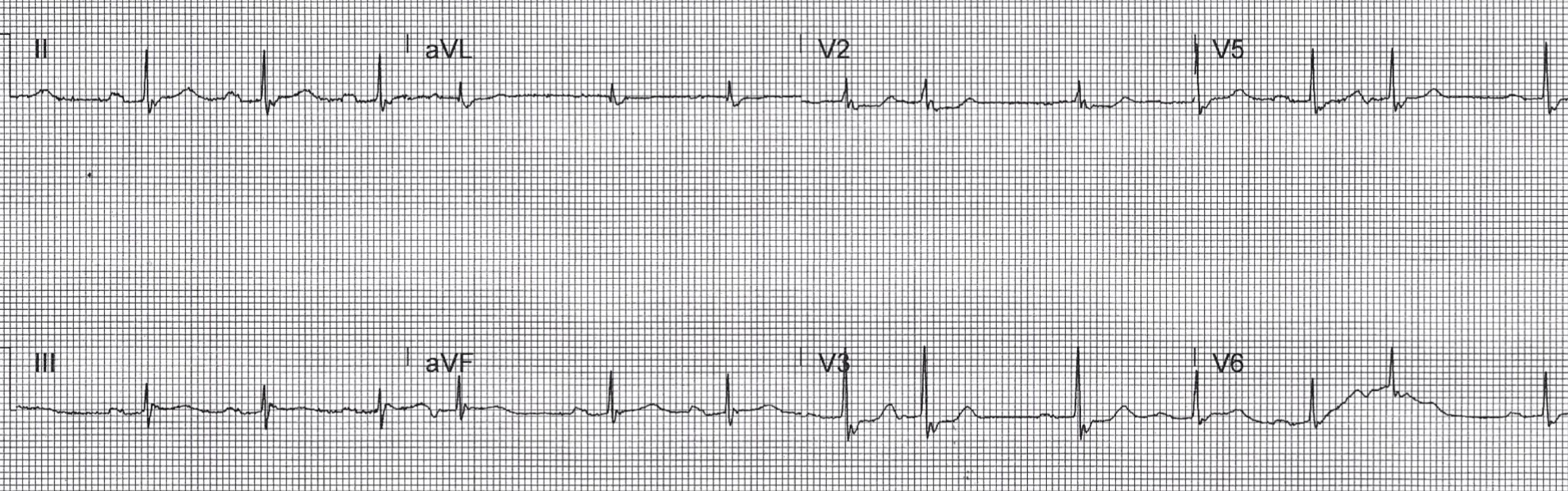
Computer read: NSR, first degree AV block, PAC, RBBB
My Read: pseudo-normalized T-waves = reocclusion in the inferior leads, and ST depression in V2/V3 concerning for posterior extension of the MI
CASE CONCLUSION:
Cardiology paged with initial ECG with concern for OMI and then with each subsequent ECG and each troponin result (levels were 40, 250, 2400) but he would not take patient emergently to cath lab despite patient also having a BP in the 90’s and refractory chest pain. The next morning the cath showed a 100% RCA occlusion. Peak troponin was >5,000. EF was 35% in the cath lab with hope that it would improve from recovery of stunned myocardium. Diagnosed with an NSTEMI rather than a missed OMI; hospital data will not show that there was a delay to cath lab activation.
Case lessons:
- Indications for emergent cath include more than just STEMI criteria. They also include hemodynamic instability or refractory chest pain thought to be due to cardiac ischemia, both of which this patient had.
- Know OMI criteria (AKA STEMI equivalents)
- Normally a RBBB has slight ST depression in anterior leads, so even subtle ST elevation there that would usually be considered “normal” can represent OMI.
- We can’t cath the patient but we can advocate for them and keep calling the cardiologist back. The problem is once they have said no to an initial request for cath, they are likely to stay with that plan to avoid having to explain a delay to cath.
- When cases like this are categorized as NSTEMI it hides the error and works against improving future performance.
