About the EM Logic Podcast:
The EM Logic Podcast focuses on recent EM literature as well as common pitfalls in emergency medicine such as confusing a cause with a coincidence, being reassured by false negative tests or getting burned by illogical assumptions. The main goal is to improve diagnostic skills in order to minimize diagnostic errors or delays. The podcast can be heard by clicking here or searching “EM Logic” on Apple podcast or “Pregerson” on Spotify. If you would like to be suggest a topic for a future episode or be considered as a guest, contact Dr. Pregerson at Safetydoc@gmail.com.
Dr. Pregerson finished EM residency in 2000, been a medical writer since 2004, and reviewed over 200 medical malpractice cases since 2008. He earned the top score on the 1999 national EM in-service exam, is the author of three peer-reviewed EM pocket references, the editor of EMresource.org and EM1minuteconsult.com, and an author at EM News. (http://bit.ly/BradyCardiaEMN.) Check out his weekly EM case challenges on Facebook (ERpocketbooks.com) & Twitter (@EM1MinuteGuru), usually each Wednesday
****
Video Intro #410: Hey ER docs. Want to never be blamed for providing inadequate aftercare instructions or forgetting to include information about incidental test results that may have important long-term health consequences? Want to minimize the chance that your patient stays home when they need to return to the ER or minimize the chance that someone is injured after an MVA where a sedating medication that you prescribed may have played a role.
In episode 41 of the EM Logic Podcast I am going to cover pearls & pitfalls plus literature & logic on Aftercare Instructions.
Episode 41: Aftercare Revisited
- Literature:
- Article: Discharge instructions for emergency department patients: what should we provide?
- EM Logic Episode 30: Abdominal Pain Red Flags & Discharge Logic
- Macro: Link to the one I use
- Return Precautions: Return precautions are your safety net, and since no doctor and no test is perfect (something I often tell patients), the verbal and written aftercare you provide are a critical safety net if things don’t go as planned. I have seen a huge variance in what providers write for the free-text part of aftercare instructions, from a phrase or two all the way to almost an entire page. The show notes on EM News will have a link to the open source documentation macro that I myself use.
- Follow-up: Can’t tell you how many med-mail cases I’ve seen where the follow up said see your doctor in 5-7 days or 1-2 weeks and the patient got worse the next day and pointed to the ACI as the reason they didn’t seek follow up sooner. There is never a reason to write follow up in any more than 1-2 days or better yet “tomorrow “. Another issue is the routine “follow up with your doctor” when the ER doc has no idea if the patient has a PMD.
- Imaging incidentals, abnormal labs and BP: nodules, cysts, old strokes, aneurysms, gallstones, etc. Tell the patient, give them copies of the imaging report and the images on CD, tell them to follow up and mention all this in their aftercare. This can be a big medicolegal risk with a long statute of limitations. Many patients have high BP or glucose and low K+. Sometimes these are just due to adrenalin/stress but sometimes they are on their way to complications from undiagnosed conditions. Make sure to stress follow-up and even initiate treatment in some cases.
- Sedating Meds: Not just for opiates and benzos and not just for driving. Also for antihistamines and most nausea medicine and/or taking a bus or walking home could be risky. Malpractice usually doesn’t cover third parties that your patient injures. Don’t rely on the pharmacist labels and pamphlets.
- Verbal Aftercare: Patients might never read your printed aftercare, so make sure you emphasize the key points verbally during your exit interview. A simple statement that “detailed verbal instructions were given to the patient in addition the written instructions” can also be a life-saver when the plaintiff will inevitably testify that the doctor never told him/her anything before discharge.
- Always Give Odds: This may be the most important part. If patients get worse instead of better most don’t want to return for the same thing that they were just sent home for, and often won’t until they are very ill. To emphasize the importance of returning if not improving, I tell patients I am sending home that there is a 5-10% chance they will get worse and need to come back, and that if I thought it was higher I would try to admit them. I think this makes them more likely to return when they should and also less likely to blame you if they do. For high risk conditions I typically estimate a somewhat lower error risk of 1-2%. Such conditions typically include cardiac, PE, stroke, meningitis. I use the 5-10% error risk for things like most abdominal pain, infections, kidney stones, etc..
Outro: Thanks for listening. If you learned something useful, please share with your peers. And don’t forget to check out the EM-News website for our show notes and links to articles and other web resources from the program. Finally, check out the free content at ERpocketbooks.com, where I have aftercare macros and so much more to share.
****
NEXT EPISODE: Episode 42: Resuscitation
- Literature:
- Recent (2025) Article: Occult Ventricular Fibrillation Visualized by Echocardiogram During Cardiac Arrest
- Classic (2016) Article: Emergency department point-of-care ultrasound in out-of-hospital and in-ED cardiac arrest
- Dose VF study: Defibrillation Strategies for Refractory Ventricular Fibrillation
- Prior Episodes: Episode 24 focused mostly on heads up CPR and avoiding CaCl and HCO3 & Episode 22 on hypokalemic arrest
- EM 1-minute Consult: NA but can check out the ACLS/Resuscitation section of Practice Changers or the 8 in 1 ED Quick Reference
- Summary of Findings:
- REASON study: A Retrospective Observational Study From the Real-Time Evaluation and Assessment for Sonography—Outcomes Network
- 1-2% of PEA and 1-2% of Asystole had V-fib when checked by bedside echo
- In ACLS always take a look with echo and if you see something reversible or shockable then treat accordingly
- DOSE VF study: RCT with survival increasing from 13% to 30% with dual sequential electric defibrillation (DSED)
- REASON study: A Retrospective Observational Study From the Real-Time Evaluation and Assessment for Sonography—Outcomes Network
- Bigger lessons & EM Logic:
- “Trust no one. Double check everything.”
- Trust no one: No test or finding is 100% reliable: pulse check not reliable, asystole or PEA may also sometimes be unreliable
- Double check: may be wide to use US to confirm rhythm
- Papers from Episodes 24
EPISODE OUTLINE ARCHIVES
Intro Video #38: Dr. P here, your friendly emergency medicine expert and podcaster. Want to learn more about the dangers of tracheal intubation and how to avoid them? This month’s episode of EM Logic focuses on intubation and what you can do beforehand to prevent triggering a subsequent cardiac arrest. (I will try to link below to the podcast but here is the title and icon)
Episode 40: Testicular Torsion
- Literature:
- Recent Article: Testicular Torsion – StatPearls from NIH
- Larry Mellick Article from 2014 ABEM Reading List: Torsion of the testicle: it is time to stop tossing the dice
- Other Article: Testicular Torsion in the Emergency Room: A Review of Detection and Management Strategies
- EM 1-minute Consult: UROLOGY
- Summary of Findings:
- Epidemiology: Peak age 13-14y w/ 67% 12-16y, neonatal peak also. (Epididymitis peaks age 19-35 so if you are diagnosing it in a boy under 16, slap yourself)
- History: Sudden >gradual testicle, flank or abdominal pain. Vomiting in only 30%. Intermittent in (unstable angina of testicle)
- pitfalls: 50% atypical: intermittent:40% >trauma:20%, dysuria:5% >abdo pain only, gradual onset
- Exam: Lost of cremasteric reflex: 70/70, high or horizontal lie, swelling:70, hard, fever:15
- detorsion: Light traction then open book (correct direction in ~2/3) unless traction spins it other way, May need to detorse up to 720° . May need to try opposite direction
- Success: decreased pain and/or testicle drops. Failure: pain same or worse
- Scores: TWIST Score (MDcalc). I’m not a fan. Low: D/C home, Mod: image, High: call Urology
- Tests: Tests are only for equivocal cases: if high suspicion call urology early to get to OR
- UA: Pitfalls: WBC:10%, abnl:30%
- Duplex: Only 85% sensitive: misses intermittent
- Normal in 10%: intermittent torsion, 180° torsion, infants
- False flags in 35%: reactive hydrocele >reperfusion epididymitis (increased flow after detorsion)
- Treatment: Manual detorsion, surgery (call urology stat), (ice may prolong viability if can’t detorse). Missed torsion still needs surgery to protect the other testicle
- Med-Mal: #3 in teenage males. “Epididymitis” is the diagnosis on the chart in 61% of settled malpractice cases. 14 year old story
- Pearls:
- “Too young for a drivers license is too young for epididymitis”
- “A useless test is better than a useless testicle” DETORSE IT
- After reperfusion the US may show hydrocele +/- reperfusion epididymitis
- Bigger lessons & EM Logic:
-
- Don’t be fooled by false negative tests. Compare to UA or TIA
- Treat without tests in acute ischemia: compare to STEMI and stroke. Don’t wait for troponin or MRI
- Beware of anchoring to an erroneous diagnosis: epididymitis in torsion, intoxication in CVA, anxiety in PE, gastritis in unstable angina
-
Episode 39: ECG in ACS
- Literature:
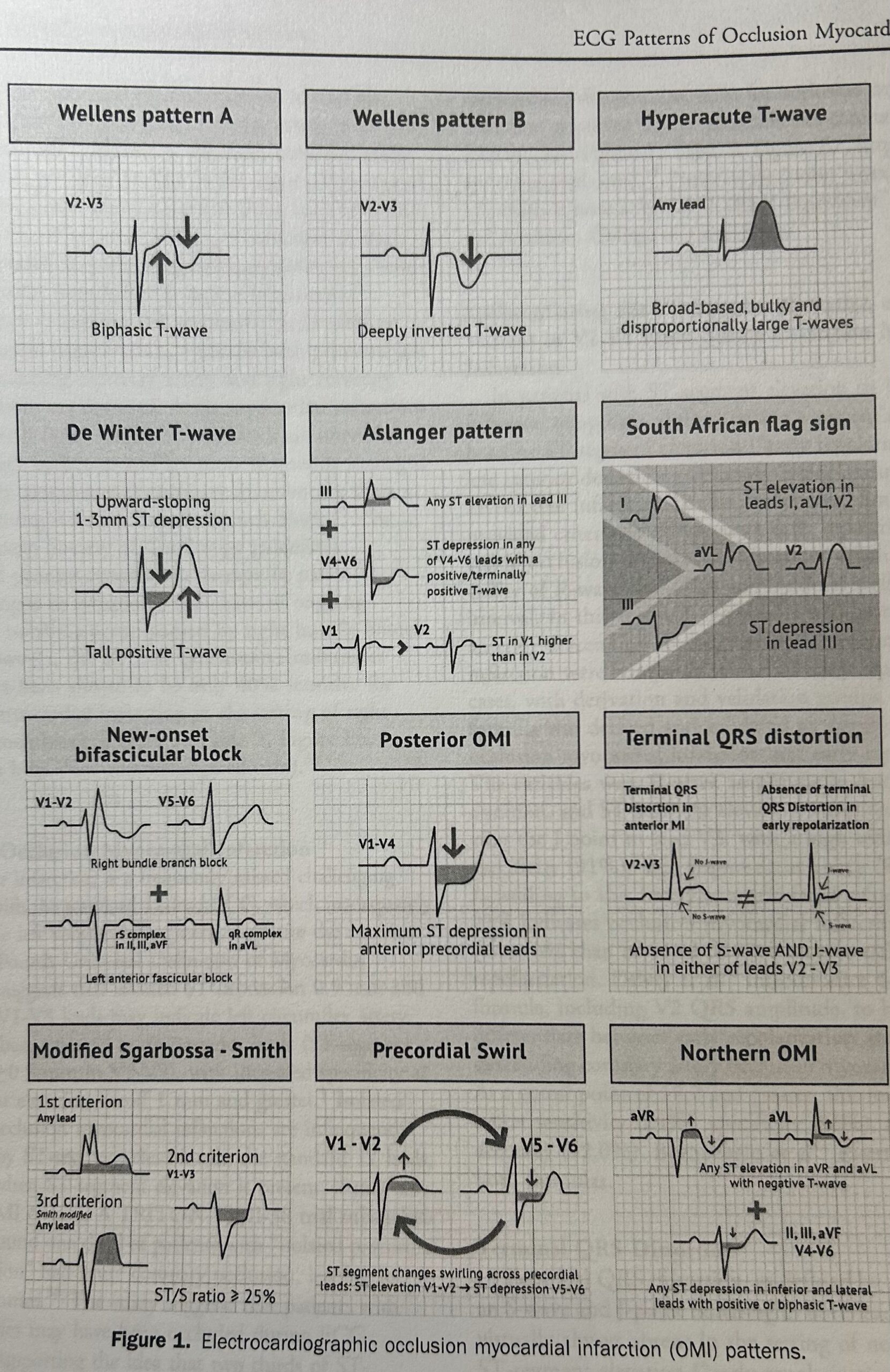
- Article: ECG Patterns of Occlusion Myocardial Infarction: A Narrative Review
- EM 1-minute Consult chapter: https://em1minuteconsult.com/?page_id=377
- Scope of the problem
- About 1/2 of occlusion MI’s (OMI) are missed by STEMI criteria
- 1/4 to 1/3 of NSTEMI’s are actually missed acute coronary occlusions, which would be best treated with emergent reperfusion. Many of these are patients who are “better” but not pain free after nitrates and so actually have refractory pain, even if it is milder pain that what they came in for.
- About 1/3 of occlusions will spontaneously open by the time of angiogram.
- ECG Patterns to master
- Best if you go to EM News website to see the visuals while listening. Rights/permission link
- Bigger lessons & EM Logic:
- Ongoing anginal symptoms is suspicious for ongoing ischemia
- Nitrates are OK but opiates may mask ongoing ischemia so avoid if you think it could be ACS pain
- STEMI criteria are neither sensitive nor specific for coronary occlusion (OMI) and miss 1/3-1/2 of OMI
- Delayed cath is OK if the event is over (ECG better, angina gone) as the artery has flow
- Emergent cath is needed if artery is still closed even if no STEMI: refractory angina, ECG criteria above, (shock)
- We need to be ECG masters because we need to advocate for better treatment for our patients when no one else will
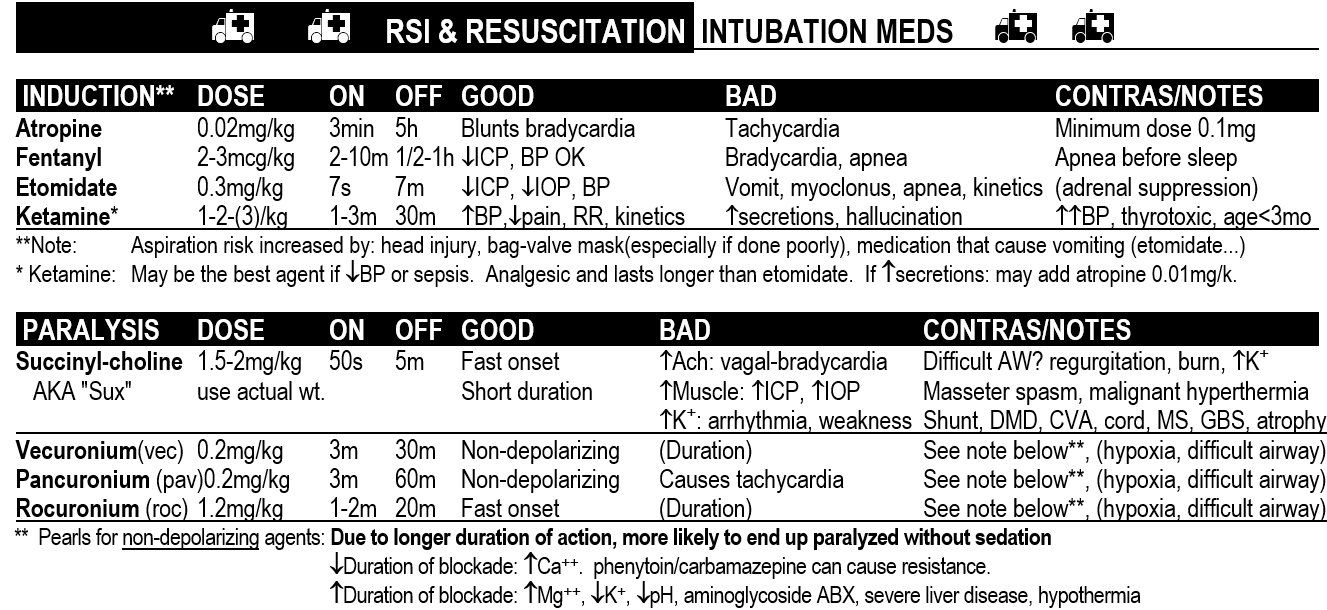
Episode 38: Resuscitation before Intubation
- Articles: Thanks to Tamara Elliot, Tri-City ED Nurse Educator
- Summary of Findings
- Scope: post-intubation hypotension in ~20% with cardiac arrest in ~2%
- 1st study: meta analysis of 44 articles in ED or ICU: 15% of intubations had hypoxia, 18% had hypotension and 2% had cardiac arrest.
- Risks for bad outcome: low BP, hypoxia, propofol use
- 2nd study: retrospective of 6983 patients.
- Risks for cardiac arrest (2%): lower BP, higher HR, higher lactate, pulmonary edema
- Bigger lessons & EM Logic:
- My Northridge ETCO2 story
- Hypotension: suppression of sympathomimetic tone, change from negative to positive pressure:
- Acidosis: decreased respiratory drive, paralysis,
- Solutions:
- Try to get BP >120/80 before intubating,
- Induce w/ ketamine or give paralytics 20 seconds before paralytics to avoid prolonged apnea (EM Quick Hits podcast episode #62)
- Use apneic oxygenation
- More:
- Powerpoint education for nurses (and docs): Peri Intubation Arrest Slides courtesy of Tamara Elliot, Tri-City ED Nurse Educator
Episode 37: Hyperacute T-waves
- Articles: Hyperacute T-waves Can Be a Useful Sign of Occlusion Myocardial Infarction if Appropriately Defined, Stephen W. Smith, MD
- Dr. Smith’s ECG Blog is a must to follow
- Summary of Findings:
- HATW: bulky, increase area under curve, more symmetric and longer QT than normal T-waves, “inflated” or “bulky”
- Should be measured relative to R wave in same lead
- QT prolongation is earliest ECG finding in OMI
- Sometimes in OMI R waves shrink more than T-waves enlarge, but either contributes to the T/QRS ratio
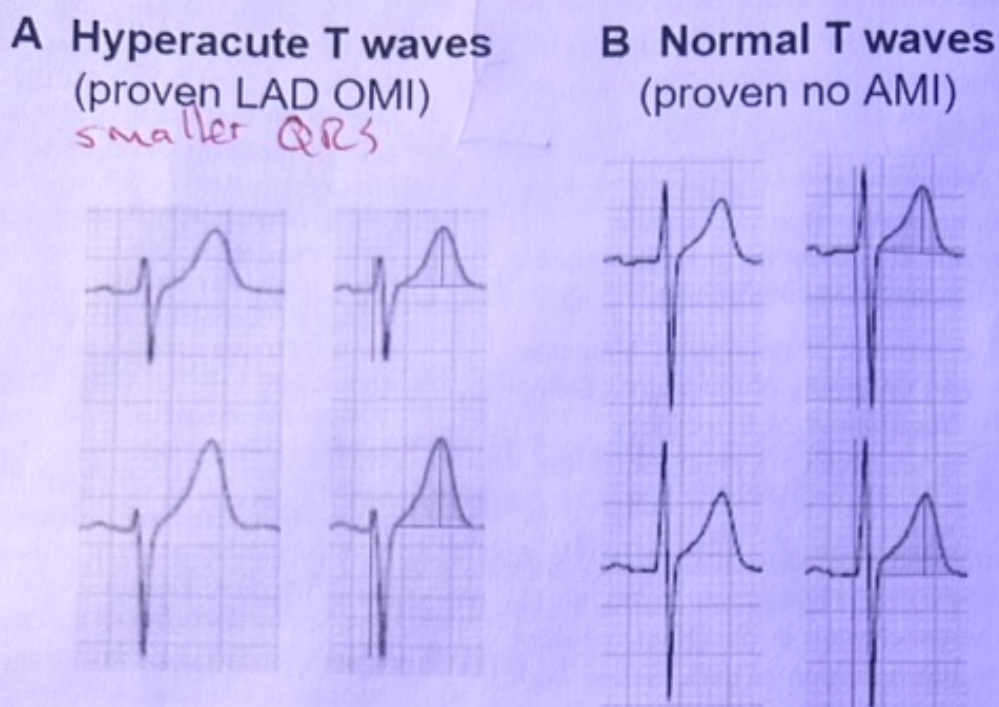
- HATW typically means myocardium is still viable/salvageable
- T wave amplitude alone is not adequate
- Bigger lessons & EM Logic:
- ECG findings can be subtle. Look hard in patients with a concerning clinical presentation
- Dynamic ECG changes are critical to look for when the chest symptoms started within the past 2 hours or whenever it changes significantly. Not every patient needs serial ECGs, but the patient with active or changing chest pain does
- An improving ECG or improving troponin can still be a big red flag if it matches the timing of the patient’s symptoms
- A stable ECG from a prior visit can be a red flag depending on why the patient had the prior ECG. Often it was for chest pain.
Episode 36: SVT
- Articles:
- The Role of Troponin Testing in Patients with Supraventricular Tachycardia, Systematic Review and Meta-Analysis: LINK
- Included 7 studies with 500 patients total. Only one study was prospective
- Summary of Findings:
- 80% of SVT patients have a troponin ordered
- Troponin elevated in 46% of patients
- 25% of SVT patients get admitted
- MACE in 6% overall, but 11% in those with elevated troponin, however follow-up duration up to 3 years
- MACE w/in 30 days: 1 study, w/in 3 months: 1 study, w/in 3 years: 2 studies, Not reported: 3 studies
- Conclusion: troponin not routinely recommended in SVT. Not a good predictor of MACE (use other criteria)
- OK to order troponin selectively; consider using the HEAR part of the HEART score to decide
- Bigger lessons & EM Logic:
- Test creep: more and more testing with no improvement in patient outcomes, sometimes leading to unnecessary admission and/or invasive studies
- Use logic and common sense when deciding who needs a troponin.
- If all symptoms resolve once SVT terminated, risk is much lower.
- If multiple cardiac risk factors AND chest pain could consider it a failed stress test
- Extend this to other conditions/tests
- More: SVT conversion
- Diltiazem better than adenosine for SVT: diltiazem is easier, better tolerated and more successful
- 98% v. 87%, no doom-like side effects
- https://em1minuteconsult.com/?page_id=360 page 16 near the bottom
Episode 35: Vital Signs
- Article:
- Can I Discharge This Adult Patient with Abnormal Vital Signs from the Emergency Department?
- Evidenced based medicine paper reviewing other studies on abnormal vital signs in ED patients and adverse outcomes
- Brit Long, et al. JEM 2024 Nov;67(5):e487-e493. Link: click here
- Summary of Findings:
- Vital sign abnormality with at least twice odds ratio for admission within 7 days after discharge include the following
-
- SBP <=95, HR >100, Temp >99, pulse ox <92% (I slightly modified these to make easier to remember)
- Abnormalities associated with death within 7 days of ED visit/discharge
- Vitals: tachycardia, vital sign abnormalities that persisted despite treatment
- Other red flags: AMS, frequent falls, dispo change by 3rd party, malfunctioning medical device
- Vitals AT DISCHARGE associated with 3-fold risk of death within 15 days of ED visit/discharge
- SBP <90 or >180, HR >90 or <50, RR >20 or <12, Temp >100.4 or <97, pulse ox <94% (slightly modified)
- Lots of overlap so not specific nor sensitive but still important
- I use HR >90 and so does SIRS and so does this article.
- Returns for admission w/in 72h or worsening condition after admission
- HR >100, RR >20 and temp >100.4 were best vital sign predictors of above
- Returns/bounce-back to ER
- Elevated shock index predictor
- Bigger lessons & EM Logic:
- Vital signs are not just normal or abnormal, they are a continuum and the closer to abnormal they get the higher should be the level of concern, especially if they do not improve and/or do not have a solid benign explanation. Examples: normalizes, HR always that high (guy last week with flutter), BP improves with orthostatics
- Pearl for vital sign trends: triage HR and EKG HR. EKG HR usually about 15 bpm lower
- I don’t calculate shock index but closer HR is to SBP the more my level of concern
- I teach residents any temp >98.6 should trigger make you question infection if you have not already
- Same with a high normal WBC could especially if there is left shift (I use 70% PMN, but the higher the more I worry)
- Most of the data we review is on a spectrum and so should be our concern level about each data point.
Episode 34: Diagnostic Momentum
- Article:
- Article topic has a small lesson, but we will cover the bigger lesson as well
- It’s Not Cyclic Vomiting Syndrome Until Dietl’s is Ruled Out: LINK
- Summary of Findings:
- Recurrent abdo pain is often diagnosed as CVS, IBS or abdominal migraine – all diagnoses of exclusion
- Dietl’s crisis may presents similarly and is due to intermittent hydronephrosis from stenosis at the UPJ, often congenital.
- POCUS may make the diagnosis, esp if patient is still in pain, which may resolve by time of formal imaging
- Treatment is pyeloplasty
- Morbidity: recurrent pain, unnecessary testing, nephron loss
- Bigger lessons:
- Confirmation bias, anchoring and/or diagnostic momentum can contribute to misdiagnosis. Likely #1 or #2 cause (false negative testing)
- Prior diagnosis or impression may be wrong – always consider this, whether an established diagnosis or a triage impression
- Even if there is a chronic condition, this does not protect the patient from a new condition. Examples: migraine & stroke, COPD & PE
- Always inquire if any symptom unusual for a patient with a chronic conditions. Ask “Are you having any symptoms you’ve never had before?”
- Also ask “Have you ever had these symptoms from another condition?”
- LOGIC: do they need a workup for a new condition? If no new symptoms and respond to therapy probably not. If not, probably so
- Diagnoses of Exclusion: AKA a DOE – The may sound cute but these DOEs bite. You may want to re-listen to episode 9
- GI: IBS, gastritis, CVS
- Neuro: AMS from drugs when actually CVA, AIDP when actually SEA
- Chest: anxiety, GERD when actually ACS or PE
- Leg: sciatica when actually acute limb ischemia
- Above all get the diagnosis right:
- It doesn’t matter if you give the perfect treatment if you have made the wrong diagnosis
Episode 33: Literature Bias
- Definition of bias: The introduction of errors into a study that distort results in a non-random way.
- Going to cover some of the most important ones alphabetically.
- Important to say that is the medical research definition of bias. In common English it means having your mind made up beforehand (cognitive bias). Thanks to Jerry Hoffman, MD Professor Emeritus, UCLA School of Medicine for reviewing this topic with me in preparation for today. He’s a giant
- Comparison bias: Control group is inappropriate. i.e. subtherapeutic dose of competitor drug
- AKA Straw man comparison
- Hawthorne effect: The study itself causes improved medical care and better results in both groups.
- Doctor’s and/or patients know they’re being watched, so they behave differently/better.
- Outcome bias: change the outcome you are looking for if the first one doesn’t work.
- Change the primary outcome for a secondary outcome. Often shows up in results and discussion.
- Publication bias: Negative studies often not published (~85% of pre-registered and 94% from industry). Meta-analyses magnify publication bias even further.
- Amplification bias: Some studies “trend” more than others, sometimes because of funding by industry. For my growing list of important but under-amplified studies CLICK HERE
- Recall Bias: Patients with the disease may better recall what they think was the cause.
- Patients without the disease may have poorer recall of a potential causal event. Mostly in observational or retrospective studies.
- Selection bias: Study population is selected and not like your ED patients.
- AKA Referral bias as it is most notable in referral populations (like in a specialist’s office)
- Spectrum bias: Early/mild disease presentation is less likely to have a positive symptom, sign or diagnostic finding.
- Notable exceptions: larger PE’s less likely to cause pain. Same with GI bleeds. Why is that [HIT PAUSE]
- Sponsorship bias: Industry sponsored studies more likely to be positive than non-industry studies.
- THIS IS HUGE: One should be very skeptical about any sponsored study
- AKA Commercial bias: deliberately introducing biases that help a company get the answer they want.
- Workup bias: Some patients never get a gold standard test (only by the test being studied)
- Thanks again to Dr. Hoffman. Below are links to some of his research and a video lecture on reading medical literature
Episode 32: Triage EKG
- Background
- Guideline for ECG to be read w/in 10 minutes of chest pain presentation
- Extended to SOB, weakness, abdominal pain…
- Frequent interruptions of EM physician
- Each time we are interrupted it takes time to get back on track and the chance of errors or omissions are increased
- Interruption to work flow:
- Provider Perspective: interrupts work flow, annoying, stressful when already busy, techs interrupt or hover.
- EMT/Tech Perspective: docs sometimes rude, snap at them, make them feel bad, slows their work flow to search for a willing provider.
- Overall: increased stress, decreased job satisfaction, decreased productivity, increases errors
- Computer EKG Reads:
- Current Quality: uses STEMI criteria with lots of false positives and false negatives. “Programmed by plaintiff lawyers”
- A.I. solutions: may be the wave of the future. Sensitivity for OMI: Queen of Hearts AI: 81%/94%, STEMI criteria: 33%/98%, Experts: 73%/96%
- EM Physician EKG Reads:
- Providers likely better than current computer algorithms but quality variable depending on knowledge base
- Resources to improve your skill: ECG weekly, Dr. Smith’s ECG Blog
- Literature:
Episode 31: Ultrasound in Aortic Dissection
- Articles:
- Summary of Findings:
- JEM study: 35 retrospective patients with AD and adequate images on bedside ED US. 86% had at least one positive finding
- AEM study: 44 prospective patients with AD and adequate images on bedside ED US. 93% had at least one positive finding, specificity was 91%
- Compare this to trans-thoracic echo by echo tech, which is: ~70% sensitive
- Parasternal View:
- Look for pericardial effusion (“large” one present in 36%). Even if small signifies high risk of decompensation & death.
- Look for for ascending aorta >3.5-4 cm (present in 70%) [root >4cm or 3.5cm inner wall w/in 2cm of valve]
- Look for a dissection flap (present in 54%) in the retrocardiac aorta.
- Image samples: https://www.erpocketbooks.com/er-ultrasounds/aortic-ed-ultrasounds/
- Suprasternal View:
- Probe in the notch and rotate in orientation of aortic arch.
- Harder to see in normal aorta. Easier to see in dissection as aorta dilates to be closer to surface.
- Image samples: https://www.erpocketbooks.com/er-ultrasounds/aortic-ed-ultrasounds/
- Abdomen & Groin:
- Abdominal aorta – we are used to imaging. Look for dissection flap (present in 54%)
- Femoral artery – not in studies but never gassed out and most dissections go into one of them
- Benefits:
- Doesn’t exclude AD but expedites care: prioritize empiric meds, CT and calling surgeon
- Risk stratification: tamponade present or not?
- Study limitations: many patients but few dissections so confidence intervals wide.
Episode 30: Abdominal Pain Red Flag & Discharge
- Article: Nothing good for a topic this specific. Based on my experience with bouncebacks/lawsuits. A lot should be common sense but also represents common errors.
- Misses:
- Are you missing something dangerous? unstable angina, AAA, perf, sepsis, SBO…
- Is your diagnosis flimsy? UTI with equivocal UA, AGE w/o legit diarrhea, gastritis w/o tenderness
- Above are DOEs – Diagnoses of exclusion. If you make them should have a fairly perfect fit
- Red Flags
- Hx: Pain off midline and/or constant. Recent surgery. Bounceback visit, esp if a new pattern. (Check CT to admission ratio)
- Exam: Concerning vitals (including weight loss or temperature >99F unless diarrhea) or rebound/rigidity
- Tests: high CRP, bands, anion gap, “physiologic” free fluid in a man or on CT…
- Rx: Pain requiring narcotics
- Green Flags
- Pain intermittent or improving w/o narcotics (unless c/w unstable angina)
- Pain clearly relieved by non-narcotic medications: antacid, antiemetic, IV fluid, pyridium…
- Pain generalized as opposed to one quadrant (not always)
- Significant watery non-bloody diarrhea (legit diarrhea)
- Return precautions: have a macro
- Recheck for surgical process: 8-12 hours or next morning if not improving
- Sooner if worse or red flag for surgical conditions
- Aftercare macro: https://www.erpocketbooks.com/documentation/
- Prescriptions: no opiates or NSAIDs
- No opiates: with rare exception, even gallstones. A last dose before DC OK though
- No NSAIDs: This should be part of the HPI for upper abdo pain and be re-emphasized at DC
- Pepto-Bismol: Has aspirin and turns poop black. I’m not a fan. Not sure what it does
- Generally OK: Tylenol, Zofran, antacids
- Antacids: H2-blocker or proton pump inhibitor for healing, Tums or Maalox for short-lived relief
- Anti-spasmotic: Consider for intermittent lower abdominal pain
- Side effects: for PPI’s – headache, hypoMg, hypoK
Episode 29: Delta Troponin
- Article: 2022 ACC Expert Consensus Decision Pathway on the Evaluation and Disposition of Acute Chest Pain
- HS Trop Characteristics
- Upper limit of normal (ULN) differs by manufacturer (and gender)
- Must be detectable in >50% of normal patients & vary by <10% at ULN
- Coefficient of Variation: reproducibility of test for same sample. Must be below 10% at ULN
- Biological Variability: change over time w/o ACS – maximum is 80% over 24h
- Delta Trop:
- Troponins rise more slowly in persistently occluded arteries than in ones that reopen.
- Change >20% definitely significant but at low levels smaller changes may still represent ACS
- It is recommended to use assay-dependent absolute change as it is more specific
- Depending on assay, a rise of just 3-5 pg/dL may be important
- Need to know values for your shop, but look at ANY rise with suspicion
- If trop is rising REPEAT ECG (if ongoing sx <2h you should have already done this)
- Dropping: if the timing is right, a significant drop can be worrisome for a resolving MI
- Single Trop
- I have heard lectures that say single trop is adequate in most patients but beware!!
- If >3h from peak symptoms AND level is UNDETECTABLE then no need for delta trop
- Which Assay do you have? My Shop: Beckman Coulter.
- If 2h delta HS-Trop <5 pg/ml MI ruled out: use HEART score + judgement to make disposition
- If 2h delta HS-Trop >20 pg/ml MI is ruled in
- Delta of 5-20 is borderline and requires admission, cardiology consult or 3rd trop
- Unstable Angina:
- Even HS trop will not typically turn positive
- There was rumor that HS trop would pick up even unstable angina, but this is not generally true
- Renal Failure Patients & Baseline Troponins
- Hospitalist often try to block admission by saying the elevated troponin is due to ESRD
- My experience: most ESRD patients have a normal troponin
- What matters is if it is different from the patient’s baseline regardless of ESRD
- May need to see what they were in the ER for last time
Episode 28: Body Temperature
- Article: Body Core Temperature Assessment in Emergency Care Departments
- Two tympanic thermometers underestimated temperature by an average of 0.8 & 1.8°C. That’s 1.4 & 3.2°F
- A forehead thermometer actually overestimated core temperature by 0.9°C (1.6°F)
- Ear and forehead thermometers not reliable if you really want to know the temperature.
- What is a Fever: Oral >37.5°C or >99.5°F, Rectal >38.0°C or >100.4°F. Axillary >37.0°C or >98.4°F. Link (top of first page).
- Seems like most people run in the 97°‘s not the 98°‘s so be wary of any temperature, even if only 37.1° or 99.0°. Though it doesn’t meet the definition of fever it still may signify infection
- Providers seem more likely to not notice a temperature unless it hits 100.0° F
- Fevers are transient so believe measured temperature at home
- If patient denies fever, ask about chills. Some people with infections only feel chills, not fever
- Fever and Heart Rate:
- Temperature rise of 1° F increases HR by ~10 bpm
- Heart rate often goes up first, some times hours before
- Recent case: 5 y/o with vomiting after falling down stairs. Had HA but normal neuro exam and persistently tachycardic. Viral? No fever for >5 hours. Did labs and fluids. 39.3°C six hours later.
- Hypothermia:
- Mostly from exposure but can be from sepsis or other causes: tox, thyroid/endocrine
- Many thermometers bottom out at 84°F
- So if your patient is 84, get a low reading thermometer or place a Foley with one and start warming them.
- Other Vital Signs: Pay attention. Vital Sign Decoding.
- Trends of gradual worsening but still “normal” vitals can be an important omen. Don’t miss them!
- Shock index: Link (middle of page 361). Basically the closer the HR gets to the systolic BP the more you should worry and if the heart rate is higher than BP, really worry!
- If febrile recheck HR once temperature normalizes
- If you want more detail on this listen to episode 20 again.
Episode 27: Acid-Base
- A different approach: in med school and residency we start off knowing both the ABG and the bicarb results and work from there. On a shift we start out with the clinical picture, the respiratory rate and the serum bicarb. I am going to go over a logical approach to finding the cause of metabolic acidosis or alkalosis.
- Low bicarb: this is the first value we get that should make us consider and acid/base issue. If it is low the first thing I look at is the anion gap.
- High anion gap: There are various mnemonics, the most famous being MUD PILES. And you should go through these but the next LOGICAL step is to order additional labs. I use the mnemonic ASK-L for that: ABG, Salicylates, Ketones and Lactate. Consider VBG instead of ABG and if overdose possible consider adding an iron level. Dehydration alone does not cause acidosis as many people echo. It can be associated with fasting and a starvation ketosis or hypotension and lactic acidosis however.
- Normal anion gap: The mnemonic I use for this is DRAFTS: Diarrhea/Diamox, RTA, Aldactone, Addison’s, Fistula (GU/panc), Tachypnea/TPN, Sepsis. The most common of these are most likely causes are hyperventilation or diarrhea. Hyperventilation/tachypnea is usually from pain or anxiety but can also be from sepsis or PE or other dangerous stuff. Sepsis can cause both gap and non-gap acidosis. The potassium level can sometimes used to help narrow the DDx.
- K+ low: diarrhea/laxative, RTA types 1-3, Diamox/meds, pancreas fistula, tachypnea/sepsis
- K+ high: urologic obstruction, RTA type-4, Addison’s, sulfur/chlorine, Aldactone
- K normal: NaCl infusion, TPN, neobladder
- High bicarb: I consider the clinical picture: Are they a COPD patient with chronic CO2 retention? Are they on a diuretic or vomiting a lot? The most common causes are CO2 retention or a contraction alkalosis from vomiting or over-diuresis
- Urine-Cl <10: diuretic, vomiting/NG tube, CO2 retention, cystic fibrosis, antacid abuse
- Urine-Cl >10: low K+, high Ca++, low albumin, Cushing’s/Conn’s/steroid, Bartter’s, Liddle’s, refeeding
- Article: Severe Multifactorial Metabolic Alkalosis in the Emergency Department: A Case Report
Episode 26: Rabies
- Rabies: I think we over-prophylax – my opinion. There are risks and costs to that. Facts/data from the EM 1-minute Consult pocketbook
- Rabies Disease:
- Rabies is rare: about 2-3 cases/year in entire US
- Incubation: 12 days-7 yrs
- Symptoms: fever, HA, paresthesias, dysphagia, pain/itch, encephalitis, dysautonomia
- Treatment: a single unimmunized patient has survived with ketamine, benzos, ribavirin & amantadine
- Rabies risk: Most important: debride, scrub with soap & water, irrigate with betadine. Do not suture.
- Risk level: see CDC website or call local veterinarian or public health for risk advice or necropsy
- Note: infected animal usually ill-appearing: paralytic >furious. Can observe 10 days or necropsy
- Pets: Healthy & can observe: no vaccine if animal well for 10 day observation period
- Looks ill or from abroad: vaccinate
- Escaped/missing: consult public health, no US human cases from a dog since 1994
- Livestock: cattle, sheep, horse…: low risk, manage similar to bite from pets
- Wildlife: bat >racoon, mongoose, skunk, fox…(<1% rabid, but likely higher if ill/aggressive)
- If animal safely captured, PEP may be delayed for testing (bites to head/neck more urgent)
- Licks to intact skin, touching or handling blood/urine/feces: do not require PEP
- Bat: unless bite/scratch marks, baby found crying or bat was found near bed, PEP not required
- Small: squirrel, rabbit, small rodents, birds, reptiles: vaccine not indicated unless aggressive
- Risk level: see CDC website or call local veterinarian or public health for risk advice or necropsy
- Vaccine: Rabies IgG 20 IU/kg at bite site + Human Diploid Cell Vaccine 1ml IM day 0, 3, 7, 14, (28)
- Risks: anaphylaxis, esp if egg allergy (RabAvert), serum sickness (JEM article link), 3 more ER visits
- Benefit: depends on the exposure. In my opinion>75% of vaccine series not indicated
Episode 25: Stroke
- Posterior Circulation: 2023 article in Journal of EM
- Posterior: ~1/4 of strokes but missed 2x as often as anterior. Mimics other things with sx like: vertigo, HA, vomiting, coma
- Vertigo: divide into spontaneous or triggered (not same as exacerbated by) and resolved/episodic or ongoing/constant
- HINTS +: adds hearing (I also add Hallpike). HINTS can be >90% sensitive for CVA but often misused.
- Head impulse test: only if ongoing vertigo to see if it is peripheral (corrective saccade only in one direction)
- (Hallpike): only us if vertigo fully resolved (triggered upbeat torsional most common)
- Hearing: rarely affected unless central cause, video with patient’s phone: can replay if nystagmus lessens or resolved
- Nystagmus: can be subtle, get in close,
- Skew: simplest, cover uncover test
- TPA: for posterior circulation lower risk of bleed and potentially longer treatment window
- Anterior Circulation:
- Less likely to be missed unless receptive aphasia or severe expressive aphasia.
- Severe aphasia, especially receptive aphasia can mimic intoxication, if thorough exam not done
- Can also mimic coma if severe: my two young female cases
- Legal cases: blamed on marijuana, alcohol, cough medicine after CT negative. CT rules out bleed, not stroke
- If patient can’t follow command, rely on painful stimuli and reflexes for motor exam
Episode 24: ACLS
-
- CPR/Defib: Anything that compromises Good CPR & early defibrillation can make things worse
- Minimize interruptions: most of us know and do this. watch your compressor, real-time feedback devices can help
- Heads up CPR: seen rarely, Korean study, decrease ICP, increase cerebral blood flow, better results in observational study. LOGIC
- ETCO2: end-tidal CO2 feedback can help CPR quality, as can O2 sat. LOGIC. ETCO2 underestimates ABG value by ~5
- Pad Position: pad position critical. Look where placed. Stacked or double simultaneous out; vector change or double sequential in
- Intubation: In general AFTER ROSC. CAB
- CCR – Cardio-Cerebral Resuscitation: There is enough oxygen in the blood for 5-10 minutes unless you suspect a respiratory arrest
- Even BVM can lower venous return: often done too aggressively. Compressions with apneic oxygenation enough for first 5-10 min (medics)
- Heads Up Intubation: Better pre-ox, better if fluid in airway, 13% fewer complications, better view, less aspiration, better if ICP or obese
- Medications: help little if at all and may harm
- Epi: If using epi, give early. Outcome worse w/ each minute of delay. Same with any intervention. LOGIC
- Bicarb: since 2010 class III (not recommended; may cause harm) in most situations. Why are so many still using it? (over 35% in 2020 study)
- Pros: volume expansion, acidosis can impair cardiac contractility. 2023 study had positive results but big potential biases & retrospective
- Cons: decreases oxygen release and SVR, worsens/causes hypokalemia, distracts from useful care, hypocalcemia
- Calcium: since 2010 class III (not recommended; may cause harm) in most situations. Why are so many still using it?
- COCA study had 50% worse neuro outcomes at one year but with wide confidence intervals. Was an RCT
- Selected Articles
- CPR/Defib: Anything that compromises Good CPR & early defibrillation can make things worse
Episode 23: Steroids
- Background: Steroids have been used to moderated a variety of severe infections despite being known immune suppressants.
- Best known: strep throat, meningitis, and more recently COVID with hypoxia.
- Less well known but evidence supported: pneumonia and labrynthitis (NEJM study years ago that no one talks about).
- Logic: Steroids for infection is logical as long as 1.) the patient is on appropriate antimicrobial therapy and 2.) the infection is at least moderate in severity.
- Steroids in pneumonia: I have been using for years. There is some new data on this.
- Cochrane review: 2017. Conclusion: NNT 18 to prevent one death in ICU admits, no mortality benefit but morbidity benefit in admitted non ICU patients.
- Side effects: hyperglycemia but not GI bleed
- Reference
- CAPE COD study: 2023 NEJM, multicenter, France, 800 ICU pts, RCT placebo vs. 200mg/d hydrocortisone infusion for ~7d.
- 5.7% absolute drop in mortality at 28 days, 5.4% at 90 days
- Limitations: ~85% of patients were excluded (influenza, aspiration, fungal, TB, already on steroids, septic shock….). Stopped early (can overestimate benefit).
- Side effects: glucose and insulin use higher but not GI bleed or other serious
- Reference
- ESCAPe study: RCT for 40mg solumedrol/d in ICU VA pts. No statistical difference in mortality, but there was a trend (2% and 3% at 60d and 180d) to improvement. Took 6 years for someone to finally publish it then since, not amplified (publication bias for positive trials)
- Problems: enrolled up to 4d after admission, poor enrollment (wanted 1,400 but gave up at 586 pts), lowish dose of steroids (is it?)
- Reference
- Pitre Meta-analysis: 2023 and includes CAPE COD and ESCAPe
- Benefits: reduce mortality in most severe CAP. Reduce ICU and duration of stay in less severe but admitted cases.
- Decadron 6mg/d or equivalent for 7 days likely best dose. Equivalent to 32mg/d of Solumedrol or 160mg of hydrocortisone
- Hyperglycemia only real side effects
- Reference
- Guidelines & Take-home: Are mixed with some societies recommending against ROUTINE use. This may change with the new studies. I will continue to use in admitted pneumonia. Risks seem low. Also good data for COVID pneumonia.
Episode 22: Hypokalemic Arrest
- Hypokalemic cardiac arrests frequency: I have never had a patient arrest from hyperkalemia or in any of the malpractice cases that I have reviewed. But, I have reviewed at least 3 malpractice cases where the patient likely died, at least in part, from hypokalemia. Risk of death and treatment of hyperkalemia is heavily amplified by lectures and literature. Maybe my experience is atypical but I have never had a patient with a hyperkalemic arrest however I have had a few of my own patients try to die from hypokalemia and still remember two of my colleagues who have had the same thing while I was on shift.
- Code during a psych eval
- Empiric treatment for hyperkalemia in a renal patient then potassium came back low
- Elderly lady with diarrhea saved by cardiac thump
- DKA patient who got insulin before K and had a K = 1.8.
- ECG Changes from hypoK:
- T-waves: Flat T, inverted T, down-up T with ST depression
- U-waves: U-wave/long QT (not really long QT but long QU), TU fusion (camel-hump T, Himalayan-T)
- Rhythm: PVCs >small P, AV block, A-fib, junctional >V-tach >V-fib/torsades (higher risk if low magnesium, heart disease or taking digoxin)
- Treatment of hypokalemic arrest: usually VT or VF. Hard to treat than hyperK due to fear of rapid IV potassium and nursing protocols. Typical IV: 10-20mEq KCl in 100ml NS over 1h in addition to PO. Crashing IV: 40mEq/h, 10mmEq over 5-10 min = 2mEq/min, or 20mEq/2-3m, (ECMO)
- Life-threatening Electrolyte Abnormalities, Circulation, 2000 – outlines aggressive K+ repletion options
- ECMO Support for hypokalemia-induced cardiac arrest, JOEM, 2015 – an even more aggressive treatment
- Hypokalemic Cardiac Arrest, Emergency nursing, 2022- outlines aggressive repletion from nursing angle
- Hypokalemia-Induced Cardiac Arrest, Cureus, 2023 – a pt who kept coding despite attempts at K repletion
- Don’t add nails to the coffin: Medications that can be fatal in a patient with severe hypokalemia or hypokalemic arrest include the following:
- QT prolongation: often given in the ER – Zofran, Reglan, compazine (Benadryl OK), many psych meds, amiodarone
- Drops serum K+: bicarb (class III in ACLS since 2010), dextrose, insulin, albuterol, epinephrine (in this paper by K+ dropped by 0.8mEq/dL with a low dose epi infusion)
Episode 21: Blood Thinners
- Background: we all know blood thinners increase the risk of ICB. There are many classes of blood thinning pills: antiplatelet agents, warfarin and NOACs are the main ones. Each class has a different risk profile. Over the years I have read lots of literature on the topic and seen different practice patterns for single CT to 6h repeat CT to admitting all of these patients. My take of the literature to date: antiplatelet agents increase risk of acute but not delayed bleed, warfarin and DOACs increase the risk of delayed >>acute bleed, which makes physiologic sense and admission v. obs v. discharge should be decided on a case by case basis. More on that at the end.
- Recent Literature: Recent paper adding to extensive literature on this topic: Delayed intracranial hemorrhage after head injury among elderly patients on anticoagulation seen in the emergency department. Reference link. warfarin risk of delayed ICB makes sense (1%) than NOACS (0.5%). Retrospective cohort study of 69,321 patients age >65 from 2016-2018: 84% no thinners, 4% were on warfarin and 12% were on a DOAC. 1.0% of all patients had a delayed intracranial
- Older Literature: Always important to consider. Does new literature fit? What are the methods? (here retrospective but 69K patients). DOACs & warfarin: early bleed: ~10% (2x no thinner), later bleed: 1-5%, death/OR: ~0.1% . DOAC risk ~½ warfarin (likely due to shorter t½): ~5% early, ~1.5% late
- Logic: Why is this? My theory is that it has to do with the half life of the thinners. DOACs have shorter half life so logically the risk would be lower if it has been a while since the last dose and if they are held after the injury.
- Dispo: some authors advise 24h admit for all, others advise dispo home for most. Red flags: lives alone, night time, <6h from injury, amnesia/LOC, INR >2.5, concerning mechanism, large swelling, skull fx, persistent vomiting/pain, recent dose of DOAC. Where there is not great literature, at least use logic rather than your autopilot
- Days off after head injury: 2 days makes sense. Lessens risk of bleed but minimal risk of CVA from a-fib unless patient has had multiple strokes, metal valve or strokes when stopping in past. 3-4 days probably makes more sense if on for remote PE or DVT.
Episode 20: Vital Sign
A lot of the med-mal cases I review involve missed vital sign red flags. The main ones include the following: unexplained tachycardia, soft BP, minor temperature elevation <100.4, and mild hypoxia. Not all patients with one or more of these vital sign red flags is going to get into trouble if they are sent home, but some of them are. Let’s dig deeper
- Heart Rate: We were all taught the normal HR for an adult is 60-100, but logic and experience tells me that things are much more complicated than that. For a healthy patient a normal heart rate is more like 50-90 and really varies depending on the physiologic and emotional state. If the heart rate is in the 90’s or even high 80’s, pay attention, especially if the BP is on the soft side. They may be in compensated shock. Only 25% of PE’s have a HR >100 but about 40% have HR >90. SIRS criteria used HR >90
- Temperature: Few ER patients without infection have a temperature >98.6. A lot of people are usually closer to 97.6 than 98.6. If the temperature is 98.8 or higher pay attention. It may mean nothing or something depending on the clinical presentation. Also, they say with each 1 degree Fahrenheit the heart rate goes up about 10 bpm, but I don’t think one causes the other because I frequently notice the HR rise before the temperature.
- Blood Pressure: if the diastolic BP is <50 think about sepsis and early pressors if it doesn’t come up with fluids. Literature says every hour delay increased mortality.
- Shock Index: Compare the HR and SBP. Normally HR/SBP should be <0.7 (eg. BP 100 and HR 70 is potentially borderline) If the HR is approaching the SBP pay attention. It may signify compensated shock. If the HR is equal to or greater than the SBP (eg. HR 98, BP 96/55) you should really worry
- Bilateral BP: Not useful for diagnosing aortic dissection (difference >20mmHg in 40% of dissections and 20% of normals). Critical for treating BP in aortic dissection or other hypertensive emergencies as well as hypotensive emergencies. Which arm do you use? It’s a trick question. Always use the higher arm, as this is usually the true BP.
- Respirations and Pulse-ox: Tachypnea can be due to anxiety but can also be from sepsis, PE, metabolic acidosis and a number of other conditions. Also remember that oxygen is more likely to do harm than good in a patient who doesn’t need it. Oxygen can cause vasoconstriction, can cause lung damage, and can lead to CO2 narcosis in susceptible individuals. In general, titrate to O2sat of 92-96%, except for COPD use 89-94%
- Pediatric Vital Signs. Fortunately most EMR’s will now flag abnormal vital signs for age. Nevertheless you should have a resource you check or formula you use, especially for the heart rate. I use 165 -s 10(age) and the following webpage: https://em1minuteconsult.com/?page_id=2124
Episode 19: IV & PO Contrast
- PO contrast: Used to be pushed for more by radiologists, but we used science, logic and persistence to limit its use. This is because it causes delays, which can be sometimes be risky or even deadly (story). Also patients with abdominal pain and vomiting don’t like it. PO contrast is rarely needed in the ED unless worried specifically about a anastamotic leak. Contrast induced bowel distention can be helpful for colitis at times. If questions, consult a surgeon.
- IV contrast
- nephropathy: fear based on observational studies in sick admitted patients. Controlled studies show it was just sick patients not the IV contrast. (Reference: Sinert R 2012 Academy E M & McDonald RJ 2013 in Radiology). Also, modern contrast is safer. Take-home: No significant risk of kidney damage in most patients with CrCl >30. Logical: try a dry CT first to see if you get a diagnosis. May miss vascular diseases and early inflammatory diseases.
- Risks: Renal: GFR <30ml/min, proteinuria, age >70y, dehydration. Meds: NSAIDs, diuretics, ACEI, pressors. Diseases: Multiple myeloma, cirrhosis, HTN, CHF, DM (even with nl GFR), sickle cell…
- Triage medicine: IV contrast often causes delays in ED throughput. Consider dry CT unless worried about vascular issues, patient very thin or symptoms for <12 hours.
- Metformin: “Stop metformin for 48 hours” is in no way logical and I have seen at least one patient die from this advice. The correct advice is: stop metformin until recheck of creatinine in AT LEAST 48 hours later. Only restart if Cr <1.4 3-5d later. Creatinine rise starts within 48h; peaks 3-5days; usually back to normal by 7-10d
- Newer: CrCl <30: stop metformin because they shouldn’t be on it. CrCl >60: OK to continue metformin. CrCl 30-60: hold metformin, see PMD to retest
- Aftercare Macro: go to https://www.erpocketbooks.com/emresources-free/documentation/
- You received IV contrast for the CT scan we did today. On rare occasions IV contrast can cause damage to your kidney. This usually is not detectable for at least 2 days and if it occurs it usually resolves within 2 weeks.
- Many health care providers falsely believe that after IV contrast you only need to stop metformin for 48 hours. This is incorrect. If you are told this, you should ignore it.
- You can take your metformin today, but after that do not take it until your doctor rechecks your kidney function and tells you it has not worsened. This blood testing should be done 3-5 days from now. Taking metformin with decreased kidney function can be deadly.
- Call your doctor today or tomorrow for more advice and to see if he or she wants to start you on a substitute medication for your diabetes for the time being.
Episode 18: Viral Infections
Before we start todays episode, my goal at EM logic has always been to share some lessons I’ve learned over the years with the EM community. However, another hope was that people from the lay community, future potential patients, would also subscribe and listen and become more informed both about potential pitfalls in medicine, such as false negative and false positive test results, and become better advocates for their own healthcare as well as become better able to care for themselves at home. Today’s episode on viral infections is one that I think should be particularly useful for laypeople and so I am asking each of you to share it with at least one of your friends or family members that does not work in health care.
- The viral battlefield: So I think the Covid pandemic and all its debates made me think a little more logically about viral infections. They are not all or none phenomena and that is why there were not always clear cut answers about masking, vaccines and other sometimes controversial topics. A viral infection is a battle between a virus and your immune system. Think of it like troops lined up on the battlefield. It is a quantitative event not a qualitative event meaning that it is not if you catch a virus or not but rather what matters is how much virus you have in your body as well as your immune system’s response that determines how sick you get or how contagious you become.
- The immune response: Prior immunity, whether from a vaccine, a prior infection, or both can lead to an asymtomatic or mild infection. These people are contagious but less so and exposures to them may lead to mild or aymptomatic infections as well.
- The spectrum of disease: Lack of prior immunity or a high initial inoculum of virus leads to more typical and severe infections. Contagion and test sensitivity usually peaks day 3-5 of symptoms, which is probably day 7-10 after infection for most viruses although this can vary. If your inoculum or exposure is limited by factors such as a brief exposure, one or both people wearing a mask or an outdoor setting, then you are more likely to have milder disease.
- Duration of illness: depending on all of the factors above you may be sick for a few days or a few weeks. A successful immune response usually takes about 3 weeks to eradicate most viral infections, but that may be much shorter when you have prior immunity. Interestingly many unexplained symptoms that people have also often go away after 1-3 weeks, so logically many of these may unknowingly be viral.
- Thinking like a detective: It is critical to do this in order to pick out cases that don’t fit the typical pattern of a viral illness that likely requires no testing and treatment other than time and one’s immune system. Some of these red flags that you may be dealing with a condition that requires further testing include the following:
- Duration: Fever lasting more than 4-5 days, illness lasting more than 3 weeks or still worsening after 2 weeks
- Atypical pain: unilateral and/or persistent pain as opposed to midline and intermittent pain
- Vomiting w/o diarrhea: has to be real diarrhea. If none DDx includes meningitis, pyelo, torsion…
- Breathing: shortness of breath, bleeding or other atypical viral symptoms
- Vitals: unexplained tachycardia, shock index >0.7
- Exam: unexpected tenderness
- Labs (if ordered): left shift (especially without leukocytosis), acidosis (sepsis can also cause non-anion gap acidosis), unexplained hyponatremia or hypoalbuminemia, any other abnormal labs, esp if new
- The first four red flags above, which are symptoms rather than exam or test results, are what I often used for return precautions given to patients on their aftercare instructions. Link to DOCUMENTATION MACRO page
Episode 17: Urinalysis
- My UA stories and the logic behind them
- Diabetic sent to chest pain unit for chest pain and UTI. She had a fever of 103.0. Correct Dx: spinal epidural abscess. Logic: look for a unifying diagnosis
- 4th visit for a man in his late 20’s with recurrent pyelo. No PMH but h/o IDU. Correct Dx: discitis. Logic: men in their 20’s rarely get pyelo without a reason
- Young woman with HA + fever + vomiting. UA showed 0-5 WBC, few bacteria, o/w negative. LP negative. Urine culture: >100,000 cfu of E. coli. Logic: safer to do the LP if usure
- 5 y/o boy with suprapubic pain. Tender on exam. UA 50 WBC, no bacteria. Correct Dx: appendicitis. Urine culture negative. Logic: boys rarely get UTI’s after age 1y and rarely tender from cystitis
- Friend of mine dx’d with SP pain. Dx: UTI . Correct Dx: appendicitis. Logic: lower abdominal tenderness w/o urinary symptoms not likely UTI
- Young woman dx’d with HA and vaginal pain. Dx: UTI . Correct Dx: HSV2 with meningitis. Logic: HSV2 may have no rash especially when systemic
- Young man treated with dysuria after unprotect sex. Dx: STI treated for GC/chlamydia. Correct Dx: HSV2 with meningitis. Logic: HSV2 may have no rash especially when systemic
- The urinalysis can be a ship for fools: there are many components and each has false positives and false negatives. Therefore if you don’t use logic you will be missing true UTI’s that need treatment as well as diagnosing UTI’s while missing the actual diagnosis. Can you say “wastebasket diagnosis”?
- Normal: <3 RBC, <5 WBC, <5 epithelial cells (some use <10 for women), occasional hyaline or epithelial cast
- Leuk Esterase: ~80% sensitive & ~65% specific for UTI. Misses 20% of UTIs
- Nitrites: ~30% sensitive & ~95% specific for UTI (typically E.coli or Klebsiella) Specific!
- pH >8.0: vegetarian, UTI (often w/ organism resistant to Macrobid)
- WBC >5: ~80% sensitive & ~60% specific for UTI. Also misses 20% of UTIs
- RBC >3: If RBC >WBC in UTI consider kidney stone. In kidney stone up to 10-20 WBC can be normal but data varies
- Bacteria: ~50% sensitive & ~90% specific for UTI. If bacteria and symptoms usually UTI. My LP UCx story
- WBC casts: pyelo, nephritis
- Summary of this and more on page of 59 https://em1minuteconsult.com/?page_id=2459
- Does the clinical picture fit? Patients often put too much value in test results. Physicians need to know better. There is a long DDx for pyuria and a false positive UA can be a dangerous red herring. The logical physician always asks “Could this be a red herring?” and “Am I missing something more serious?”
- WBCs DDx: Some of the more important ones: STI, epidural abscess, discitis, appy, psoas abscess, diverticulitis, papillary necrosis, fistula
- Bacteria DDx: contamination, colonization of Foley. No treatment if no symptoms unless pregnant or renal transplant pt (granulocytopenia, pre-op GU)
- Epithelial cells: if high, repeat the UA unless you are very confident. You will often be surprised.
Episode 16: Pain Medicine
- Duration of action: Duration of morphine is 5 hours and for Dilaudid is 4 hours (last letter in the name)
- Side effects:
- Apnea: Fentanyl >Dilaudid >morphine. Higher risk if alcohol or sedatives on board, elderly, COPD, OSA/obesity
- Nausea: 10%, vomiting 3% antiemetic prn only
- Constipation: 10%, stimulant laxatives best, Oxycodone may have less
- Death: IV Morphine peaks in 40min, IV Dilaudid peaks in 20min, IV Fentanyl peaks in 10min
Codeine ~1% of light skinned, but 29% of African Americans are ultra-fast metabolizers & are at higher risk of OD
- Alternatives to opiates: muscle relaxants, NSAID’s. Pyridium, Maalox, Lidoderm, prednisone, Ketamine. Ice for headache too
- It masks pain: Feeling better after narcotics should not reassure you of a benign diagnosis. If narcotics required for possible ACS should consult cardiology and push for cath lab
- Drug Seekers: so much better than it used to be. Having a department policy minimizes variance among your group and gives returning patients consistent expectations.
- Prescriptions home: Unless you have a definitive diagnosis that requires it they may just stay at home and get worse. Not for biliary colic unless very reliable.
- Cruel to be kind: avoid for undiagnosed conditions; it may delay return visits for worsening disease Avoid concomitant sedatives.
- Fentanyl: Don’t use Fentora or patches in opiate naïve patients. Don’t use unless you are VERY familiar with all of the risks
- CDC Opiate Guidelines: Non-opioids are preferred except for active cancer or palliative care. When prescribing opioids, use the lowest effective dose. state prescription drug monitoring systems. Avoid concomitant sedatives. All 12 on page 133 of https://em1minuteconsult.com/?page_id=1504
- ACEP’s Opiate Policy states opiates should be avoided for acute exacerbations of non-cancer chronic pain. All on page 160 of https://em1minuteconsult.com/?page_id=2299
Episode 15: Aortic Dissection
- Question: When should you consider a CT chest for aortic dissection? Answer: When there is chest pain plus any of the following: upper back pain, concerning BP differences, concerning CXR, other unexplained/unusual symptoms/results especially if the brain, abdomen or a leg is involved.
- Question: Which BP is the real one, the one in the left or right arm? Answer: neither – it is the one with the higher reading and really you should check legs instead of the arms as in my experience most dissections go into one of the legs but few go into the arms. My estimate is that 95% of dissections go all the way into one of the legs but only 5-10% go into an arm. Use the highest BP to guide your antihypertensive dosing
- Question: Is it worth doing a bedside ultrasound? Answer: Yes. It can expedite care. I first look for a pericardial effusion then look at the aorta as it courses behind the heart. I then look in the sternal notch, then the abdomen and finally the femoral arteries, with the last one being new for me. For a video of a recent diagnostic femoral ultrasound go to EMnews.com. Echo alone is about 70% sensitive for dissection so checking all 5 of these location probably has a sensitivity in the 80’s-90’s. If you see a dissection you don’t necessarily need to check the remaining sites
- Question: When should I do a pericardiocentesis? Answer: When your patient is hypotensive and lethargic with a plethoric face, but before they are dead. My experience is that most deaths from AD are due to tamponade and most of these people could have been saved if they got a pericardiocentesis. Currently recommendation is only 10mL at a time titrating to clinical improvement.
Episode 14: Intubation
- Bag valve mask: No one taught me this, but in a breathing patient, let the patient trigger your squeeze. I rarely see RN’s, RT’s or MD’s synchronizing their bagging with a breathing patient. In order to optimize preoxygenation and decrease complications take Olivia Newton John’s advice to John Travolta and feel your way. It’s logical.
- Upright intubation: Logical for the reasons below as well as for CPR if needed. (Korean study)
- Pro: Better pre-oxygenation & apneic oxygenation, better for blood/vomit/fluids, 13% fewer complications, better view, less aspiration
- Con: If you are short you may need to intubate from the side of the bed
- Suction Assisted Laryngoscopic Airway Decontamination (SALAD): Logical if any fluid (blood, vomit…) in airway
- Oral suction, Yankauer as a tongue depressor, scope in (keep light/lens out of vomit)
- Slide Yankauer into esophagus at L side & pin w/ L side of blade, rotate blade a bit for view
- After intubation but before first breath suction ET tube down into trachea
- Benefits of ketamine: Etomidate is fine but I’m switching to ketamine because its side effects and kinetics are more logical
- Pro: BP, no apnea, bronchodilator, onset 1-2m (safer to give before paralytic), lower risk of paralysis w/o sedation
- Con: secretions, rarely can drop BP
- Dose: 1-2mg/kg IV, onset 1-2 minutes, lasts 20 minutes
Episode 13: Hemoptysis
- Intro: Hemoptysis not common but a good place to use logic – uncommon things often are as there is not as much data.
- Minor Hemoptysis: About 95% of cases – usually phlegm > blood. Usually benign and/or bronchitis. I do a CXR and give ABX if they are coughing up blood – seems logical as more severe than the average case. Probably no studies on if ABX help this subset. Not a listed exclusion on MIPS, which include comorbid condition, ABX in past 30d, or has a competing bacterial diagnosis. For MIPS macro library CLICK HERE
- Massive Hemoptysis: Very rare – probably less than 5%. Definition no longer the amount but rather enough to cause clinical decompensation. 50-100ml can be fatal. Logic: they die from asphyxiation not blood loss. Don’t give blood – want a soft/low BP until bleeding stops. Why do you think we have the vasovagal reflex? [see episode 8 from October]
- Stabilization: Positioning is critical. Position of comfort and don’t lie flat! Exam and CXR to try to figure out if from one lung or both. If asymmetric, lie on side with bad side down. Only intubate if forced to as it doesn’t protect the airway and prevents patient from trying to clear the blood. If hand forced do upright intubation with SALAD (suction assisted laryngoscope airway decontam) and 8-8.5 ETT if possible. Permissive hypotension wise. Avoid blood unless Hb <8 or big drop from baseline
- Definitive: CXR then CT if stable. CTA chest – contrast timing for bronchial arteries (not PE timing). Reverse thinners. TXA IV and nebulized. Try to intubate the good lung. IR to embolize if find a source on CT. Bronchoscopy once stable but many or most will die. For more CLICK HERE and scroll to page 262
Episode 12: AMA Discharge
- Listen to a lecture on this topic: I’ve heard a lot of good lectures on this topic. I am primarily going to focus on things I do that I don’t often hear about in lectures or notice some of my colleagues skipping. For more advice on AMA discharge and an open-source charting macro go here: ERpocketbooks.com – Documentation Macros
- Find out their reasons: This is covered by most lecturer’s but is critical. Maybe if you know why they don’t want to stay, you can do something helpful to change their mind. At the very least, you should be charting this information as well as your response to it. Also use their reasoning to build empathy and try to understand them. This will hopefully strengthen the therapeutic alliance and increase their comfort level returning if they change their mind or are able to rearrange other commitments.
- Get others involved: The PCP is always a good resource as are family members. The PCP knows the patient better than you do and will likely be the one they are following up with. They may be able to convince the patient to stay even when you are not. If not they can help you formulate the best plan B that you can. A family member may also be able to convince or coerce the patient into staying. In addition, if the patient ends up dying, guess who is most likely to be the one suing you? Correct – the family. If the family has some ownership of the outcome they are more likely to let you off the hook. You get bonus points if you can have a family member sign the AMA form as a witness so ask your nurse to do this.
- Sign your admit chart: If there is a lawsuit later, I want my chart to clearly reflect that I was planning to admit them and never changed my mind. That is why I don’t document the AMA discharge until after I have finished and signed my chart as an admit. After I do that I add an addendum for the AMA part. I don’t want any misunderstandings about what happened.
- Send them with gifts: make sure the patient gets the safest plan B you can offer including ALL of the following when appropriate.
- A warm invitation: Invite them to return if they feel worse or change their mind. Let them know AMA discharges occur often and about 25% of people eventually change their mind and come back. This statement can make them less hesitant to return if they get worse.
- Aftercare paperwork: Do not let your nurses get in the lazy habit of having them sign a form and then leaving without aftercare instruction. Yes, AMA is more work. If they elope without aftercare instructions, document it.
- Prescriptions: I generally avoid controlled substances or anything that might mask pathology, but other medications, such as antibiotics, I almost always prescribe. Don’t take an AMA personally. It happens to all of us. Send them home with gifts
Episode 11: Lab Values
- Troponin – False negatives & False positives: Troponin will be falsely negative early in an occlusion MI, when the benefit of intervention is highest. It will also remain negative in unstable angina; the newest troponins are more sensitive but still misses true unstable angina. Troponin can be falsely positive in a variety of conditions but one should not assume this unless the level remains fairly flat on serial testing and is similar to levels from prior visits. If the troponin is significantly higher or if it rises or even only falls, this should be a red flag. Troponin-i should not be elevated simply because a patient has renal failure. Most renal failure patients have normal troponins so don’t dismiss a positive troponins simply for this reason.
- UA – meant to lead you astray: The UA can be very tricky in UTI. It can be a red herring when you don’t question pyuria when there are >5-10 epithelial cells; repeat those UA’s. On the other hand I not infrequently see UA’s with few bacteria and <10 WBC or even <5 WBC that are later proved to by full fledged pyelonephritis based on contrast CT or urine culture.
- WBC morphology – Bands, Toxic granulation & Dohle bodies: Most people know about bands but some EMR’s don’t flag them when they are abnormally high. Some EMR’s now call them immature granulocytes instead of bands. Toxic granulation and Dohle bodies are almost never flagged even though they are more specific for severe bacterial illness than bandemia. These WBC morphologic changes are taught briefly in medical school then forgotten by most. They are not very sensitive, but they are specific and sometimes are the only major lab clue when the WBC count is normal. Always wait for the dif to come back. CLICK HERE FOR MORE
Episode 10: Lab Values
- Adrenaline-Stress Tetrad: This episode will focus more on some often underappreciated interpretations or components of certain lab tests and less on logic per se. Through adrenaline/epi release, stressors such as pain or anxiety can cause 4 different transient lab abnormalities. Can you name them? They are: hyperglycemia, hypokalemia, leukocytosis and non-anion gap metabolic acidosis as compensation to a respiratory alkalosis from hyperventilation. How does each occur?
- CO2 – Metabolic Acidosis: dehydration doesn’t cause an anion gap acidosis. That’s not logical and it’s not in the famous MUD PILES mnemonic. Dehydration can actually cause a hypokalemic metabolic alkalosis and diarrhea can cause a non-gap acidosis. Lack of food for more than ~6 hours however can cause an anion gap acidosis by causing a ketoacidosis through metabolism of fat.
- CRP – Better than WBC: I like the CRP in two situations. 1) If the WBC count is elevated but I think it is demargination rather than infection a normal CRP supports that conclusion. The other is when the CBC is normal, but I think the patient is infected and may even want to admit. If the CRP is high it supports that and helps counter pushback from hospitalists that put too much stock in the CBC. You can use an ESR in addition or instead but if you only use one CRP is usually more sensitive because it rises earlier than ESR.
- D-dimer – Testing Creep: In general, you should only order a D-dimer when you think the patient needs a VQ or CTA but hope to save time and radiation. Avoid ordering a D-dimer “just in case”. There are at least two pitfalls to doing that. The obvious one is that it is elevated leading to unnecessary CT or VQ, which will slow you down, especially if you have to then explain incidental findings that occur in about 30% of chest CTs. The less common but more dangerous pitfall is that a positive D-dimer can be a red herring. If you do order a D-dimer that comes back only mildly elevated, remember there are two validated tools for using a higher cut-off:
- Age adjusted D-dimer: can be applied to patients >50 years old
- YEARS criteria: click HERE and scroll to CHEST: YEARS
- LFTs – Super high with AST >>ALT: ALT is more liver specific than AST (L is for Liver). Whenever you see very high AST and it is more than 3-4 time the ALT consider that the cause may not be in the liver. In such cases consider sending a total CK. You may be dealing with rhabdomyolysis rather than hepatitis and the CK will often be MUCH higher than the AST
Episode 9: Diagnoses of Exclusion
- Emails: I heard from a listener on last month’s podcast who wanted to share another vasovagal trigger theory he had. That listener suggested that the carotid trigger could have evolved because biting predators frequently go for the neck. That makes sense to me. If anyone wants to email me with questions or suggestions or comments, please send those to SafetyDoc@gmail.com.
- Horses & Zebras: I think most if not all of us have heard the statement “When you hear hoof beats think horses, not zebras”, which is true unless you are in East Africa. Other aphorisms include “common things occur commonly” and “rare manifestations of common diseases are more frequent than common manifestations of rare diseases”. These are all true. We should all be looking for horses first, but we should also know when the diagnostic fit is not good enough and we actually need to go on bit of a zebra hunt.
- Deer: I want to introduce another animal – DOE, a deer, a female deer, but also standing for… Diagnosis Of Exclusion. These are beasts that are actually common in the ED but are also common reasons for doctors to miss the correct diagnosis. Dangerous conditions frequently masquerade as deer. In the ED we should be very careful with these. Here are some deer to avoid:
- Gastroenteritis: this deer should present as intermittent, generalized abdominal pain with vomiting and diarrhea. The pain should not be constant nor localized and there must be diarrhea, especially if vomiting has been present for 24 hours or more. If the fit is not good evaluate for more dangerous conditions that don’t get better on their own such as pyelo, appendicitis, cholecystitis, DKA, meningitis, etc.
- Anxiety: Anxiety is perhaps the most dangerous DOE in the ED. Mimics include potentially immediate life threats such as PE, ACS/MI, aortic dissection, DKA, etc. Their symptoms can overlap significantly or completely with anxiety and the exam may not be that helpful. Also remember that lots of patients in the ED have secondary anxiety caused by whatever their primary medical conditions may be.
- Dehydration: After anxiety, dehydration is perhaps the next most common diagnoses that I see in the malpractice cases that I review. It’s fine for your patient to tell you they feel dehydrated and feel like they need IV fluids (magic water I call it), but don’t believe them unless they have vomiting or diarrhea or another ACTUAL reason to be dehydrated PLUS you feel confident they don’t also have something more dangerous
- Visit History: One other caveat on deer. Whenever it’s the first time or the worst time a patient has come to the ED for their current symptoms it makes the chance you are dealing with a deer even less likely. This is a great question to ask the patient and/or reason to do a chart biopsy. On the other hand, if a patient has had the same symptoms and been properly worked up for it recently with nothing worrisome found, then in that case it would be more reasonable to make a DOE and discharge the patient home; just be careful.
Episode 8: Bleeding
- Logic Quiz on Bleeding: The answers are within and at the end of the podcast. 1) Why are most bleeding gastric ulcers painless? and 2) Why do people have a vasovagal reflex in the first place? There are logical answers. I can’t prove they are right, but they most likely are. If you want to try to figure these out on your own hit the pause button.
- Hemostasis: First I learned about the clotting cascade. If you want to see a nice clotting cascade that includes the sites of action of various blood thinners and/or a summary chart of NOACs including reversal strategies, there should be a click here button in the show notes. Next I learned about the platelet plug. I think there is something that comes even before that: the vasovagal reflex. This reflex slows the HR and drops the BP and logically that would help the platelet plug form. Probably the best target vital signs for this reflex would be a HR around 60 and BP around 90, like we aim for in aortic dissection. This sweet spot gives the body the best chance to form a stable clot without the deleterious effects of frank hypotension. Like most other things, people are different.
- More Pressure, Less Gauze: The next logic, most of you probably already know, but your patients usually don’t and some of your nurses and techs also don’t. Lots of gauze will probably just wick more blood from a wound. Instead have the patient hold focused pressure with the least gauze necessary.
- Logic Quiz Answers: 1) Why are most bleeding gastric ulcers painless? Because ulcers that cause pain typically present before they bleed significantly. 2) Why have we evolved to have a vasovagal reflex? Probably it’s the first step in hemostasis after injury. Pain and the sight of blood are known triggers. When your heart rate and BP both drop and you lie down, bleeding has a better chance to stop. Maybe the vomiting scares some predators away and maybe that’s also why it can be linked to peeing or pooping.
Episode 7: Acute Coronary Syndrome
- First ask, “Are you having pain now?”: If your patient answers NO then consider this unstable angina until proven otherwise even if the pain went away with an antacid. Antacids relieve pain in ~15% of ACS. Why? It’s called coincidence. The real lesson here is that the percent of acute coronary syndrome that presents as unstable angina is probably 15% at a minimum. It’s actually probably at least twice that since not everyone tries an antacid. If you are looking for unstable angina you are less likely to be fooled by false negative troponins. This is still true of high sensitivity troponin although there is supposedly some literature says that says if the level is below the level of detection at least 3 hours out from peak pain and presentation it can rule out unstable angina. It has to be better than normal. It has to be undetectable.
- 2nd Troponin vs. 2nd history: I would like to be spread the following lesson to everyone in EM: “Before you do a second troponin, do a second history!” You need to really nail down the timing and duration of symptoms the best you can, otherwise you may be misled. Some patients speak their own language: “Constant” can mean “Frequent”. Most of us already know that “No medical problems” can mean “No untreated medical problems” to a lot of people. It is safest to start with the assumption that all chest pain is unstable angina until proven otherwise, that the pain is episodic lasting 5-10 minutes, and that the troponin and EKG may both be useless.
- HEART score Logic: The HEART score is super useful and can help protect you if you send the wrong patient home, but you should still try to avoid doing that. The HEART score’s major blind spot is unstable angina because if pain lasts less than 20-30 minutes, both the troponin and EKG may be normal. Another caveat of the HEART score is grouping together all the patients with scores from 0-3. If the risk of this group is about 1-2% on average, logic dictates that patients with a score of 0-1 are actually at lower risk but those with a score of 2-3 are likely at higher risk, perhaps 3-4% or even more. What is the actual risk associated with a HEART score of 3? We won’t know until someone does the study but once you hit the 4-6 score group your risk jumps to 10-20%. If you extrapolate the data, the risk of a MACE at 30 days is probably 2-3 times your HEART score, so for 3 it would be 9%, if you use logic.
- Back to the question “Are you having pain now?” If your patient answers YES then your next question should be “When did the current episode start?” or better yet, “When was the last time you had no discomfort?” If it was less than 2 hours ago you should be doing serial ECG’s every 30 minutes if you can in order not to miss a STEMI with an initially non-diagnostic or even near-normal ECG. It can take 2 hours or even more for ST elevation to manifest in some cases. You want that to be picked up early, not 8 hours later when your patient is on the floor and it is too late for cath to help much.
Episode 6: Physical Exam
- Head-Jolt sign: This is about 99% sensitive and 50% specific for meningitis. Have patients rapidly turn their head side to side. If it doesn’t hurt or they have to do it twice, make sure they don’t have meningitis. I will often grab their head and do it for them, but first definitely explain what I am doing to family members.
- Eyes-Red eyes: Consensual photophobia or limbal flush suggests iritis or keratitis rather than conjunctivitis.
- Pulmonary exam: Demonstrating how you want them to breathe and having them breathe more rapidly in and out is quicker and more sensitive for abnormal lung sounds. If you think you hear consolation when performing lung exam, ask a yes or no question. This can help continue your history, speed up your exam, and identify a pneumonia (a sort of modified egophony). After that and the end of an exhale, tell them to stop breathing and stick out their tongue (if no mask) while you listen to the heart with your stethoscope closer to the heart and without interference from lung sounds or, worse yet, speech. Bonus: Look at their tongue for hydration status.
- Vascular-Pulses in the feet: Comparing pedal pulses is critical when there is a possibility of a knee dislocation, an aortic dissection, or acute limb ischemia, all of which can be sneaky and time-sensitive. Popliteal arterial injuries often are diagnosed late due to severe leg pain or spontaneous knee reduction. Aortic dissection rarely extends into an arm but almost always extends into a leg. Acute limb ischemia can mimic DVT, sciatica, or even a stroke.
- Ortho-Pain location: Have them touch the exact spot that hurts the most. Without this and a confirmatory exam, you may end up imaging the wrong part of the spine or extremity. If you are lucky, it will only cause a delay; if you are not, it can cause a disaster. I have seen many misses or near misses due to this.
- Ortho-Arm/hand neuro exam: Have the patient make an OK sign with the wrist in dorsiflexion and third fourth and fifth fingers spread apart. This allows you to evaluate the median (C5-8), ulnar (C8-T1), and radial nerves (C6-C8) in a five-second motor exam.
Episode 5: TIA/Stroke
- CTs don’t rule out strokes: CT scans only rule out bleeds. This is what I teach my patients, my residents, and myself. This obviously goes double for TIAs. We know this as physicians, but I am surprised by the number of misses that seem to occur when stroke/TIA was a consideration, but then the CT is negative. These misses with false negative head CTs are almost exclusively in cases where the physician probably had low pretest probability for a stroke because either the symptoms were atypical or the patient was quite young. But a substantial minority of strokes are in young patients or are atypical, and these are exactly the types of strokes that CT scans are more likely to miss so it shouldn’t really alter your post-test probability that much.
- Do you have a better explanation for the presentation? I think in such cases the question to ask is, “Do I have a better explanation for the clinical presentation than stroke?” If you do and the fit is good, then it is probably logical to make that diagnosis. But if you don’t or the clinical fit is not really that good, then you should think long and hard about admitting for a stroke workup even if it’s a bit of a battle. This is especially true if this is the first time for this patient. Have they been worked up for something similar before with an admission? Beware of wastebasket diagnoses.
- Know atypical presentations of stroke/TIA: A medical student can diagnose a classic stroke or classic TIA. It takes wisdom and logic to diagnose stroke/TIA with atypical presentations such as the ones below.
- Posterior circulation strokes mimicking a migraine but with something that doesn’t fit.
- Vertigo that doesn’t fit labyrinthitis or BPPV.
- Other posterior circulation strokes: a variety of acute presentations; 2.5 times more likely to be missed than anterior circulation strokes. Blurry vision=nystagmus.
- Anterior circulation strokes that mimic intoxication with altered mental status often from expressive or receptive aphasia.
- Young patients with no known risk factors: ~10% of strokes.
Episode 4: STDs
- PID is often missed. This is because the exam can be unimpressive. You’ve probably heard of the chandelier sign. Remember >50% of men and >80% of women have no symptoms with chlamydia, so if you use your logical brain it follows many cases are very mild. In terms of risk, remember that PID is not always an STD; it is caused by vaginal flora in about 15% of cases.
- Fitz-Hugh-Curtis (FHC) is often missed. If you are not diagnosing ~1 case per year you are probably missing it. The classic case is pleuritic RUQ pain in a sexually active woman, normal LFTs, elevated D-dimer and normal CT angio of the chest. If it is from chlamydia there are almost never any pelvic symptoms (LOGIC). Incubation usually -3 weeks. Do a sexual history. If there is a new partner, consider FHC even if non-pleuritic pain. Gallstones can be a red-herring.
- HSV meningitis is often missed. Most of the cases I have diagnosed had been seen by at least one provider in the prior week. It often follows a mild primary infection that has just irritation but no rash or blistering. Since ~50% of each HSV1 and HSV2 positive patients have never had an outbreak it follows that mild cases likely occur and are missed. Meningitis can start mild and elevated CSF RBC’s only occur ~50% of the time.
Episode 3: Aftercare
- Return Precautions: Return precautions are your safety net, and since none of us is perfect, the verbal and written aftercare you provide are critical, especially if things don’t go as planned. I have seen a huge variance in what providers write for the free-text part of these, from a phrase or two all the way to almost an entire page. Mine tends to be quite long but it’s mostly a macro that I tailor to the patient. The show notes on EM News will have a link to them if you want to used them.
- Imaging incidentals, abnormal labs and BP: Lung and adrenal nodules, ovarian cysts, gallstones, etc. Tell the patient, give them copies, tell them to follow up and add them to the their pre-fab aftercare. This can be a big medicolegal risk with a long statute of limitations. More important is to know things that are not so likely to be incidental such as free fluid in the abdomen of anyone who doesn’t ovulate. Many patients have high BP or glucose and low K+. Sometimes these are just due to adrenalin/stress but sometimes they are on their way to complications from undiagnosed conditions. Make sure to stress follow-up and even initiate treatment in some cases.
- Sedating Meds: Not just driving. Even taking a bus or walking home could be risky. Don’t rely on the pharmacist. Malpractice usually doesn’t cover third parties. (link to After Care Instruction macro)
- Verbal Aftercare: Many patients never read your printed aftercare, so make sure you emphasize the key points during your exit interview. Also, most people don’t want to return for the same thing that they were just sent home for, and often won’t until they are very ill or it is too late. Therefor you have to EMPHASIZE this. I often tell people that I think their is a 5-10-15% chance they will need to come back, and that if I thought it was higher I would try to admit them. I think this makes them more likely to return when they should and also less likely to be upset with you if they do.
Episode 2: Pulmonary Embolism
- Classic PE: pleuritic chest pain, SOB, tachycardia and S1Q3T3 after starting an oral contraceptives and then going on a long flight to get chemotherapy.
- Large PE misses: about 20% of PE’s are painless and probably ~50% of the large ones are painless, but this is rarely taught. Logic is that there is collateral circulation. Large PE’s almost always cause SOB however. These PE’s often mimic ACS or sepsis due to tachycardia (rare in ACS) and/or low BP, ischemic EKG changes, and elevated troponin/BNP/WBC. If the patient is unstable a bedside echo can really help as can the EKG. Look for a dilated right ventricle on the echo. On the ECG look for a new right axis or T-wave inversion in both inferior and anterior leads as both of these are very rare in ACS.
- Small PE misses: pleuritic chest pain only. Logic is that there is no collateral circulation so there is a lung infarct, which causes pain. No SOB, normal vitals, normal EKG, no known risk factors. If you don’t have a more likely diagnosis use PERC or D-dimer. You may know the PERC, but do you also know the exclusion criteria? (link to PERC exclusion criteria)
- Too many chest CTs: for PERC, COVID is a more likely diagnosis most of the time so don’t dimer them unselectively! Logic: how many PE’s have you or your colleagues diagnosed with a mildly elevated D-dimer or when you had a better explanation for symptoms but you were just CYA? Better than logic is logic + literature: Use age adjusted D-dimer and YEARS criteria to minimize unnecessary CT. Both of these are validated and can be used in pregnant patients as well. (link to YEARS criteria) Also know the causes of false negative D-dimer (on thinners, symptoms >1 week)
Episode 1: Unstable Angina
- Therapeutic Trials: Maalox relieves pain in 15% of ACS. Why? The logical answer is coincidence, so before you order Maalox ask if the pain is already improving. Do the same for NTG and you will be less likely to get fooled by coincidences.
- Second Troponin: before you do a second troponin, do a second history in order really nail down the timing and duration the best you can, otherwise you may end up wasting time, or worse yet, giving yourself false reassurance.
- Pain Duration: assume all cardiac chest pain is unstable angina until proven otherwise and that every chest pain patient has episodic pain lasting 5-10 minutes and therefore your troponin and EKG may both be useless.
- HEART score: Not as useful if pain has resolved because troponin and EKG may be useless. Also, score grouping may overestimate risk in a patient with a score of 0-1 and underestimate risk in a patient with a score of 3. Use the info in scores but don’t blindly follow them. Apply logic.
****
PLANNED FUTURE TOPICS
Back Pain
- Make sure you are not missing thoracic pathology. Most disc disease is lumbar or cervical, but most infections, tumors and pathologic fractures are thoracic. To a patient “lower back” may include the lower T-spine (lower 1/2 of the 17 bones in the back)
- Make sure you are not missing mild weakness. Your arms vs. your patient’s legs is not a good way to test strength. Have the patient tip-toe or do single leg toe raises, walk on their heels and do 5 lunges. If they have difficulty, they may be weak.
- Check DTR’s and clonus if there are any leg symptoms. Learn to do this with your fingers for the patella and the side of your thumb for the ankle reflex
Bias Minimization
- Unconscious bias affects everyone but there are strategies to minimize it. The most common strategy is to know the types of bias that most frequently come to play in medicine and ways to mitigate each
- Anchoring bias: assuming a prior or current diagnosis is correct. This can be mitigated by talking to the patient before looking at prior notes or current test results, by being skeptical of what the patient or prior providers think is going on, especially when there is a more urgent or dangerous explanation.
D-Dimer in Unstable Angina
- D-dimer is elevated in about 62% of unstable angina while troponin is elevated in only about 5%. Logic: UA has clot formation but no infarction so this makes sence. REFERENCE:
- D-dimer is elevated earlier in MI than troponin
- other (+): Chest pain: MI, unstable angina, aortic dissection, Fitz-Hugh-Curtis, pericarditis. Other dangerous: CVA, AAA, CVT
- Cons: Overuse may inappropriately lead to imaging. Only 15-70% specific (worse age >50)
- false (–): Symptoms >1 week, (Possible: small clot, on heparin/warfarin/NOAC)
- false (+): Trauma: postop <10d, bruise. Chronic: ESLD, ESRD, CA, DM, CVD, sickle. Inflam: ID, DIC
- D-dimer-MI: Sensitivity/Specificity for ACS ~ 85%/95%, which is better than troponin & rises earlier. For MI ~95% sensitive, for unstable angina ~62% sensitive (troponin only ~5% sensitive
- Literature: https://pubmed.ncbi.nlm.nih.gov/10966534/, https://pubmed.ncbi.nlm.nih.gov/17102647/ , https://journals.sagepub.com/doi/pdf/10.1177/147323001003800523
Imaging
- If a patient is supposed to have a test done in the near future or a consult in the near future but they are worried enough to come to the ER then do the test or consult that same day if possible. If you assume it’s safe for them to wait, you may be doing so at their peril.
- Always recommend and document follow-up plan for incidental findings. Though many of these are not dangerous. Some are
Hemoperitoneum
- I was taught once that abdominal distention is due to one of the four F’s: Feces, Flatus, Fat or a Fetus, but this list does not include one of the most important causes of bloating, which is hemoperitoneum. Hemoperitoneum may be very painful to some, but feel more like bloating to others. I would estimate in a third of cases of hemoperitoneum I have seen the abdominal exam is not impressive. This is regardless or whether the cause is ruptured ectopic, ovarian cyst with excessive bleeding or a more rare entity like a ruptured splenic artery aneurysm or even cases where no cause is found.
- More important is to know things that are not so likely to be incidental such as free fluid in the abdomen of anyone who doesn’t ovulate.
Trauma Logic & ATLS 10th edition (2018) Update Highlights
- Airway: Video laryngoscopy recommended
- Breathing: Needle thoracostomy: 4th/5th intercostal space mid-axillary line (no longer 2nd space mid-clavicular)
- Circulation: Maximum of 1L of crystalloid during the initial assessment then blood if BP stays low
- IV fluid: infusion of >1.5 L of crystalloid associated with increased mortality in trauma (sicker patients?)
- Blood: early use of blood instead of large volumes of crystalloid
- TXA: 1g IV over 10 min recommended w/in 3 hours of injury followed by 1 g over 8h
- Tourniquet: recommended for severe + persistent extremity bleeding
- Disability:
- Head-Adults: anticoagulation reversal table, guidance on BP, guidance on seizure meds
- Head-Children: PECARN algorithm recommended
- Spine: Canadian C-Spine and NEXUS C-spine guidelines both recommended
- Backboard usage > 2 hours should be avoided
- prostate/rectal exam is no longer recommended unless specific indication
- Burns: Parkland formula should not be used in all cases
- Adults: 2 ml/kg/%TBSA initially then reassess
- Children: 3 ml/kg/%TBSA initially then reassess
- Electrical: 4 ml/kg/%TBSA initially then reassess
- Geriatrics: Elderly have increased mortality
- Comorbidities: 2x increased mortality if cirrhosis, coagulopathy, COPD, CAD or diabetes
- Transfers: Once need for transfer clear, expedite contacting trauma surgeon and transferring
- Avoid/minimize unnecessary tests and/or procedures that are likely to delay transfer

