For more check out EM Logic podcasts for December 2022 and January 2023 by clicking HERE
****
CBC infectious red flags
- Automated Diff: done by Coulter counter by a spectrometer. Can pick up bands, blasts and abnormal RBC morphology
- Manual Diff: Only done if ordered or there are red flags on the automated diff, which may vary by hospital. Shows WBC morphology
- NEW as of 2019: starting circa 2019 new hematology analyzer (i.e. Sysmex) reports IG = Immature Granulocytes (percent and absolute), which include promelocytes, myeloctes and metamyelocytes. Bands are not IG’s. IG% >0.4% is considered to represent a Left Shift and can signify infection, but up to 2% can be normal.
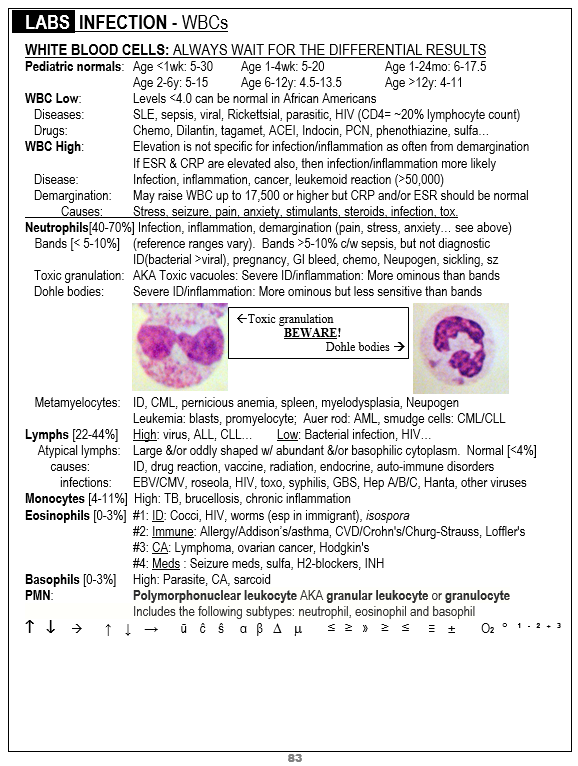
WBC morphology: toxic granulation, Dohle bodies or vacuoles are red flags for serious infection, more so than bands. Always look to see if they have been called out. Atypical lymphocytes have causes beyond mononucleosis. For these search the sample page below.

RBC morphology: Howell-Jolly bodies can signify hyposplenism, leukemia, thalassemia, or pernicious anemia and the first two of these are associated with decreased immunity. Pappenheimer bodies can signify splenectomy, MDS, sickle cell disease, sideroblastic anemia, hemolysis or lead poisoning, the first three of which can be associated with decreased immunity
WBC Demargination: my strategy for how to handle an elevated WBC count that I think is just due to demargination is as follows: These WBC counts will usually be between 11-16, although they can be higher. I order a CRP and maybe also an ESR (CRP is usually more sensitive). If the CRP is normal, I usually don’t worry about the elevated WBC count if my clinical suspicion is also low. Be a bit more concerned when the PMN count is >80% but the total WBC count is normal; this is unlikely to be due to demargination
***
Adrenaline Tetrad
Pain, anxiety, trauma, pregnancy or any form of emotional or physiologic stress can cause any or all of the following lab abnormalities, probably from endogenous adrenaline release and/or hyperventilation
- Leukocytosis from demargination (often left shift but should not have toxic granulation or Dohle bodies and CRP should be normal)
- Hyperglycemia from adrenalin
- Hypokalemia from shift into cells similar to giving albuterol for hyperkalemia
- Low bicarb non-gap metabolic acidosis to compensate for respiratory alkalosis (hyperventilation). This probably starts within minutes but is only remarkable if hyperventilation has been going on for more than half an hour (my estimate)
***
Metabolic Acidosis
Dehydration alone shouldn’t cause an anion gap acidosis. Dehydration is actually supposed to cause a contraction alkalosis. Diarrhea can cause a a metabolic acidosis but it should be a non-anion-gap acidosis. When there is an anion-gap acidosis in a GI condition it is typically due to starvation ketosis from the lack of food for more than ~6 hours leading to the metabolism of fat, which generates ketones. Typically this should not be the assumed cause in a sick patient until lactic acidosis has been ruled out
***
Super high LFTs with AST >>ALT
ALT is more liver specific than AST (L is for Liver). Whenever you see very high AST and it is more than 3-4 time the ALT consider that the cause may not be in the liver. In such cases consider sending a total CK. You may be dealing with rhabdomyolisis rather than hepatitis and the CK will often be MUCH higher than the AST
***
D-dimer Creep
In general, you should only order a D-dimer when you think the patient needs a VQ or CTA but hope to avoid the time and radiation by getting a negative D-dimer. Avoid ordering a D-dimer “just in case”. There are at least two pitfalls to doing that. The obvious one is that it is elevated leading to unnecessary CT or VQ, which will back up the department further and slow you down, especially if you have to then explain incidental findings that occur in about 30% of chest CTs. The less common but more dangerous pitfall is that a positive D-dimer can be a red herring. I have seen multiple cases where a positive D-dimer lead to a delay in diagnosing ACS and even a STEMI (11% of STEMI’s do not manifest on the initial ED ECG)
If you do order a D-dimer that comes back only mildly elevated, remember there are two validated tools for using a higher cut-off:
- Age adjusted D-dimer: can be applied to patients >50 years old
- YEARS criteria: click HERE and scroll to CHEST: YEARS
***
