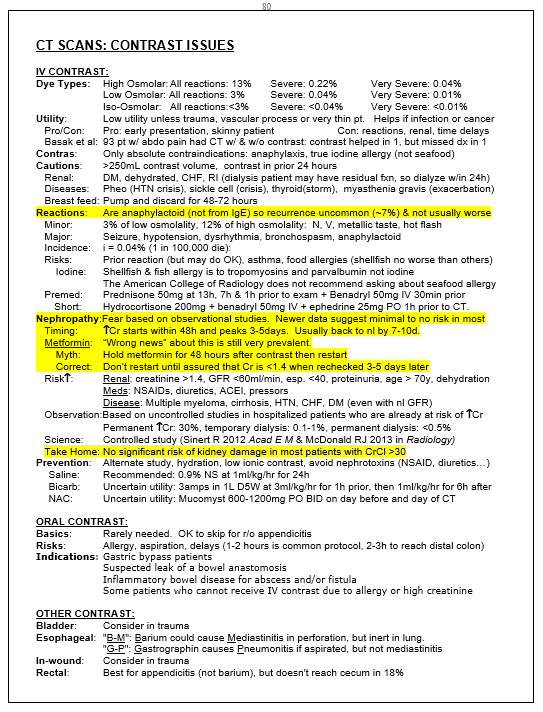
CONTRAST RECAST:
MYTHS:
- Myth: Oral contrast is often helpful
- Myth: Don’t use contrast if the patient reports iodine allergy
- Myth: A history of a contrast reaction contraindicates using contrast
- Myth: IV contrast has be shown to cause kidney damage
- Myth: Patients on metformin can restart in 48 hours after IV contrast
TRUTHS:
- Oral contrast is rarely useful, can be cruel, and has few indications
- No one is allergic to iodine
- Risk of allergic reaction is low, even in someone who has had one before
- Risk of kidney damage, if it exists, is minimal.
- If CrCl is >30 there is no proven risk of kidney damage from contrast
- Metformin should not be restarted until kidney injury is ruled out with repeat labs
For more details, see page shot below from my Tarascon book
****
RADIATION CONSIDERATION:
- Cancer: lifetime risk is up to 1 in 1000 for most torso CT’s and is cumulative with repeat imaging. Latency usually >20 years but can be 2-5 years for leukemia and 10 years for breast and thyroid cancers.
- Intellectual development: mostly in younger children
- Fetal Malformation: for pregnant patients
- Incidental Findings: occur in 15-30% of CT scans of the chest and abdomen. These are rarely important, but usually result in further downstream testing, patient anxiety and occasionally unnecessary treatments, not to mention the extra time required by you to try to explain all of this to the patient
STUDIES THAT EMPLOY IONIZING RADIATION:
- CT scan: high exposure levels
- X-ray: low exposure levels
- Nuclear Medicine: medium to high exposure levels
- Fluoroscopy: medium to high exposure levels
ALTERNATIVES THAT DON’T USE IONIZING RADIATION:
- Ultrasound: for pelvic pain, appendicitis, renal colic…
- MRI: for appendicitis in pregnancy…
- Labs: D-dimer for PE, UA for renal colic…
- Observation: at home or occasionally in the hospital
- Surgery: without CT for classic appendicitis or if US shows appendicitis
****
MINIMIZING RADIATION IN DIAGNOSTIC IMAGING: A HEAD TO TOE APPROACH:
Below are some suggestions to consider that may change your practice and protect your patients
- Brain Imaging: Consider home observation instead of CT for isolated loss of consciousness without other red flags. Read NEXUS-II, the Canadian head CT tool and the PECARN study. Consider outpatient MRI for pediatric seizure with normal neurologic exam
- Neck Imaging: Use NEXUS &/or Canadian C-spine tools to minimize imaging. Use plain films except in high-risk cases. Do not CT the neck for convenience just because the patient is going to CT for another body part
- Chest Imaging: Use D-dimer to rule out PE in low probability patients. Use D-dimer in intermediate probability patients if your lab has a d-dimer with a sensitivity of 95% or better. Do not order a D-dimer unless you were planning to do a CT or VQ already. Willy-nilly ordering of D-dimer “just in case” leads to increase in the use of CT and VQ. Use VQ instead of chest CT preferentially in younger patients with normal chest X-rays and minimal concern for serious conditions other than PE. VQ has a much lower radiation dose than CT and this is especially important in women and younger patients. It is also more sensitive (98%) than CT (83%).
- Abdominal Imaging: Use ultrasound first in younger patients or those who have had multiple CT’s. To check for appendicitis in children, start with ultrasound in most cases. Consider learning bedside ultrasound of the appendix to help you determine which formal test, if any, to order in textbook appendicitis in thinner young adults: CLICK HERE FOR BRIEF IMAGE TUTORIAL . In classic renal colic, especially with hematuria on UA, formal imaging may not be required if risk for AAA or other serious conditions is low or recent prior CT showed a normal aorta. Consider ultrasound instead if formal imaging desired, especially in younger patients.
****
The table below is helpful for comparison. Actual doses may vary
Copyright ERPocketBooks.com
****
SUGGESTED READING ON THIS TOPIC:
- Picano E. Informed consent and communication of risk from radiological and nuclear medicine examinations: how to escape from a communication inferno. BMJ. 329(7470):849-51, 2004 Oct 9.
- Picano E. Sustainability of medical imaging. BMJ. 328:578-80, 2004 Mar 6.
- National Research Council Committee of the Biological Effects of Ionizing Radiation (BEIR VII), 2005
- Kuppermann N, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet, Sept 15, 2009
Hoffman JR, et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma, (NEXUS-I), NEJM July 13, 2000– Pregerson DB. A to Z Pocket Pharmacopoeia, 2nd edition, EMresource.org, 2005– Pregerson DB. Quick Essentials: Emergency Medicine, version 4.0, EMresource.org, 2009– Pregerson DB. Cornucopia: Emergency Medicine, EMresource.org, 2009– Wells PS, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis, N Eng J Med, Sept 25, 2003– PIOPED Investigators. PIOPED, Prospective Investigation of Pulmonary Embolism Diagnosis, JAMA 1990;263:2753-2759– Turkstra F, et al. Reliable rapid blood test for the exclusion of venous thromboembolism in symptomatic outpatients, Thrombosis and Haemostasis 1996:76;1;9-11– Fedullo PF, Tapson VF. The evaluation of suspected pulmonary embolism, N Eng J Med, Sept 25, 2003, 349,13– Stein PD, et. al. Multidetector computed tomography for acute pulmonary embolism, (PIOPED II); New Eng J Med, June 1, 2006– Roberts JR. Radiographic Imaging During Pregnancy, Emergency Medicine News, Marcy-May 2002– Donnelly LF, et al. Minimizing Radiation Dose for Pediatric Body Applications of Single-Detector Helical CT, AJR:176, Feb 2001– Basak S, et al. Is Unenhanced Helical CT Sufficient for Evaluation of Acute Abdominal Pain? Clin Imaging. 2002; 26(6):405-7Stiell IG et al., The Canadian CT Head Rule for patients with minor head injury, Lancet, May 5, 2001Hoffman JR, et al. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma, (NEXUS-I), NEJM July 13, 2000
- Wells PS, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis, N Eng J Med, Sept 25, 2003
- PIOPED Investigators. PIOPED, Prospective Investigation of Pulmonary Embolism Diagnosis, JAMA 1990;263:2753-2759
- Turkstra F, et al. Reliable rapid blood test for the exclusion of venous thromboembolism in symptomatic outpatients, Thrombosis and Haemostasis 1996:76;1;9-11
- Fedullo PF, Tapson VF. The evaluation of suspected pulmonary embolism, N Eng J Med, Sept 25, 2003, 349,13
- Stein PD, et. al. Multidetector computed tomography for acute pulmonary embolism, (PIOPED II); New Eng J Med, June 1, 2006
- Roberts JR. Radiographic Imaging During Pregnancy, Emergency Medicine News, Marcy-May 2002
- Donnelly LF, et al. Minimizing Radiation Dose for Pediatric Body Applications of Single-Detector Helical CT, AJR:176, Feb 2001
- Basak S, et al. Is Unenhanced Helical CT Sufficient for Evaluation of Acute Abdominal Pain? Clin Imaging. 2002; 26(6):405-7
****