History of Present Illness:
A woman in her mid-50’s with no significant PMH, currently on Macrobid for a UTI is sent from the urgent care to the ER for suspected anaphylaxis. Before sending they gave IM epinephrine and Decadron. She complains only of SOB, which she said is no better after the medications they gave. She denies any oral, skin, GI or other symptoms.
Vital Signs & Physical Exam:
Vital signs are normal except for a pulse of 123 and pulse ox of 93% on room air.
Rales are heard at the bases bilaterally, but only with a full rapid inspiration. They do not clear with coughing or deep breathing. The resident did not hear them. There is no wheezing. It is unclear what the physician at the urgent care heard.
Labs: WBC 15, CRP 2.6 then 5.0, chem-7 normal. BNP and trop normal.
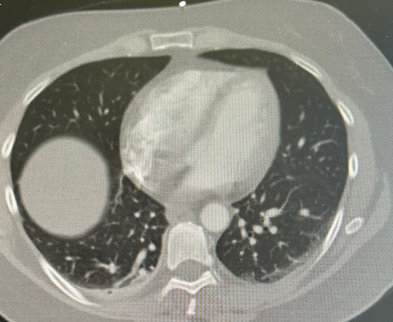
Imaging: CXR read as normal. A CT scan is done
What is the most likely diagnosis?
- A) Atelectasis
- B) Blood clot
- C) Cardiac tamponade
- D) Pulmonary fibrosis
SCROLL DOWN FOR ANSWERS & 1-MINUTE CONSULT
<<<<<<<<<<<<<<<<<<<<< ADVERTISEMENT & SPACER >>>>>>>>>>>>>>>>>>>>>
THE EMERGENCY MEDICINE POCKETBOOK TRIFECTA
Emergency Medicine 1-Minute Consult, 5th edition
A-to-Z EM Pharmacopoeia & Antibiotic Guide, NEW 5th edition (currently printable pdf only)
8-in-1 Emergency Department Quick Reference, 5th edition
******************************************************************************
<<<<<<<<<<<<<<<<<<<<<<<<< END SPACER >>>>>>>>>>>>>>>>>>>>>>>>>
ANSWERS: What is the most likely diagnosis?
- A) Atelectasis – CORRECT, TECHNICALLY. There is dependent atelectasis, which can cause rales. I wonder if this could be early pulmonary fibrosis
- B) Blood clot – ruled out by the CT scan
- C) Cardiac tamponade – ruled out by the CT scan
- D) Pulmonary fibrosis – CORRECT, POSSIBLY. Macrobid is a rare cause of pulmonary fibrosis. Early pulmonary fibrosis can mimic atelectasis. Though this cannot likely be proven, there is not better alternate explanation of why this women had hypoxia and rales on exam an elevated and rising CRP and “Atelectasis” on CT.
1-Minute Consult on this topic: Click HERE and scroll to proper page.
CASE CONCLUSION: patient’s HR improved as the epi wore off and she was sent home. Macrobid was stopped and Keflex was substituted. The medication change and the steroids helped and her SOB resolved over the next 1-2 days
CASE LESSONS:
- Subtle lung findings are best picked up by having the patient take a rapid full inspiration then expiration through an open mouth. IF you do this routinely you will pick up rales or wheezes that others have missed.
- Sometimes a zebra hunt is warranted
- When things don’t fit always consider a medication side effect. Below are some of my favorites
- Headache from PPI
- Hypomagnesemia from PPI
- B12 deficiency from metformin
