History: A woman in her mid 60’s with a history of DM and ESRD presents with frequent falls and generalized weakness for the past 3 days. She is a bit self-assertive and rude and keeps telling you to check her records and not ask so many questions
Exam: Vital signs are normal except for a pulse in the 120. Physical exam is notable for tachycardia, diminished breath sounds on the left and mild symmetric leg edema
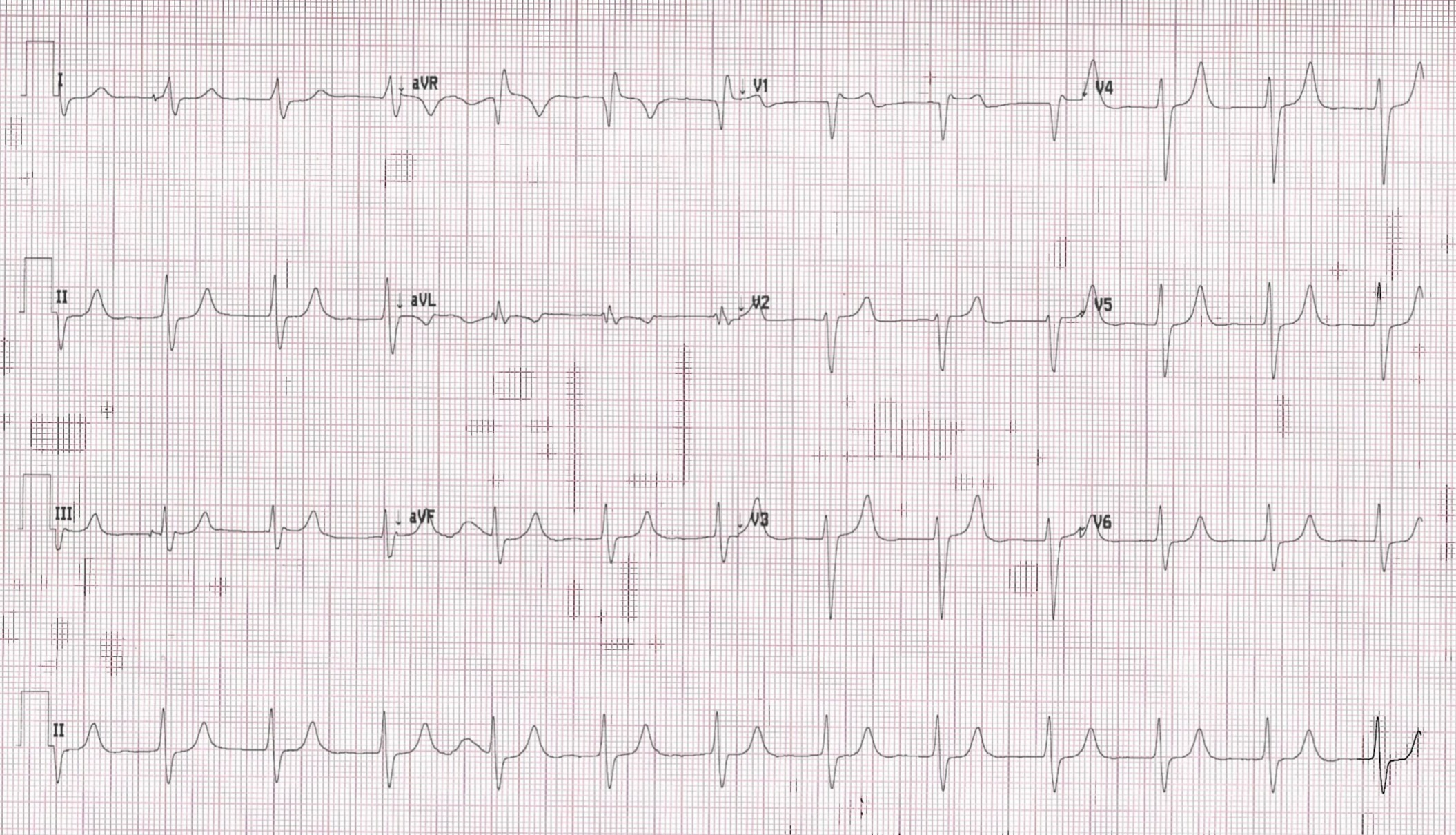
An ECG is done
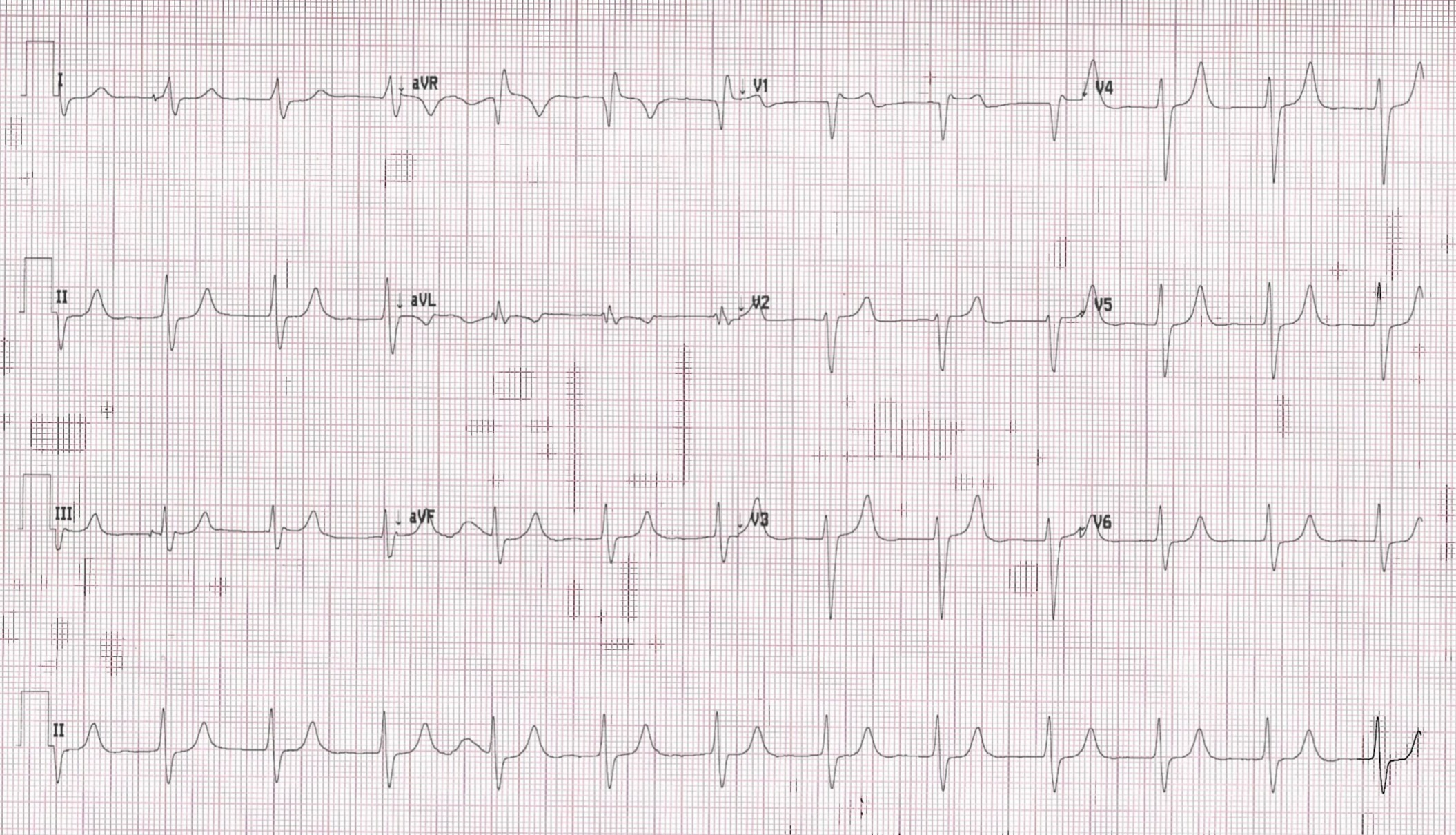
Computer Read: NSR at 74 with 1 degree AVB and IVCD
What is the most likely cause of ECG findings in this patient?
- A) ACS
- B) Electrolyte issue
- C) PE
- D) Medication issue
SCROLL DOWN FOR THE EKG ANALYSIS & 1-MINUTE CONSULT
<<<<<<<<<<<<<<<<<<<<< ADVERTISEMENT & SPACER >>>>>>>>>>>>>>>>>>>>>
THE EMERGENCY MEDICINE POCKETBOOK TRIFECTA

- Emergency Medicine 1-Minute Consult, 5th edition
- A-to-Z EM Pharmacopoeia & Antibiotic Guide, NEW 5th edition
- 8-in-1 Emergency Department Quick Reference, 5th edition
******************************************************************************
<<<<<<<<<<<<<<<<<<<<<<<<< END SPACER >>>>>>>>>>>>>>>>>>>>>>>>>
ECG interpretation: Sinus brady with 1 degree AV block and flat P waves plus narrow/spiky T-waves and a widened QRS. Each alone could be from hyperkalemia, but all 3 together in a dialysis patient is highly suspicious
QUIZ ANSWER:
- A) ACS
- B) Electrolyte issue – CORRECT. K was 6.8.
- C) PE
- D) Medication issue
Outcome: Went into 2:1 block, admitted to ICU for BRASH syndrome
Emergency Medicine 1-Minute Consult: Click here and scroll
***
