History of Present Illness: A man in his mid 70’s with a history of PVD but no known CAD presents with approximately 2 hours of non-radiating chest pain and exertional SOB.
Vital Signs & Physical Exam: Vital signs are normal. Physical exam is otherwise normal except for isolated right-sided anterior cervical/submandibular swelling
An ECG is done
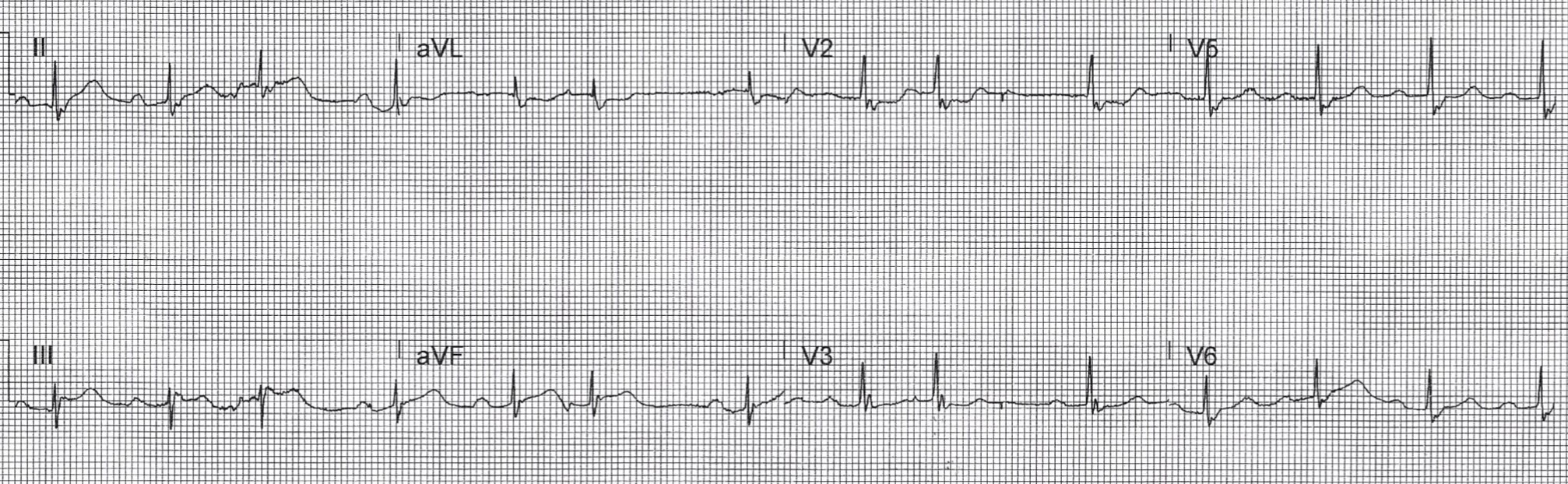
Computer Read: NSR at 80, first degree AV block, PAC’s, RBBB
What is the most likely cause of ECG findings in this patient?
- A) STEMI
- B) OMI
- C) RBBB with expected secondary ST and T wave changes
- D) findings worrisome for PE
SCROLL DOWN FOR ANSWERS & 1-MINUTE CONSULT
<<<<<<<<<<<<<<<<<<<<< ADVERTISEMENT & SPACER >>>>>>>>>>>>>>>>>>>>>
THE EMERGENCY MEDICINE POCKETBOOK TRIFECTA
Emergency Medicine 1-Minute Consult, 5th edition
A-to-Z EM Pharmacopoeia & Antibiotic Guide, NEW 5th edition
8-in-1 Emergency Department Quick Reference, 5th edition
******************************************************************************
<<<<<<<<<<<<<<<<<<<<<<<<< END SPACER >>>>>>>>>>>>>>>>>>>>>>>>>
ANSWER:
- A) STEMI
- B) OMI – CORRECT
- C) RBBB with expected secondary ST and T wave changes
- D) findings worrisome for PE
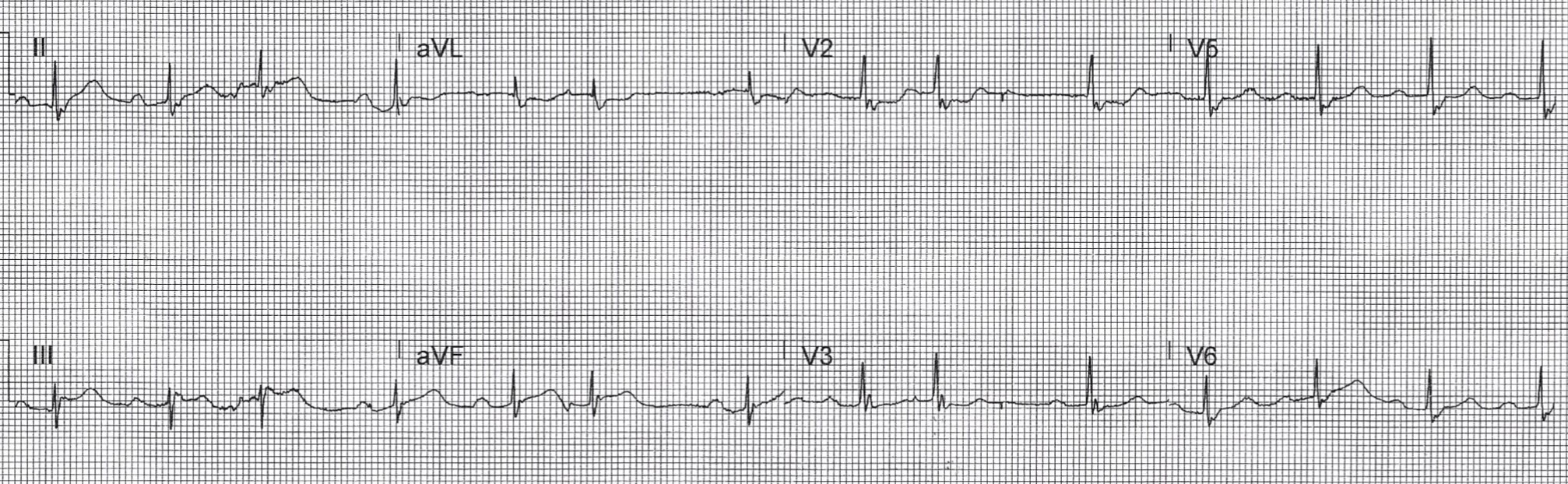
Serial ECGs:

Computer Read: SB at 54 first degree AV block, RBBB
Actual: reperfusion inverted T-waves in the inferior leads and ST depression in V2/V3 back to normal levels for a RBBB
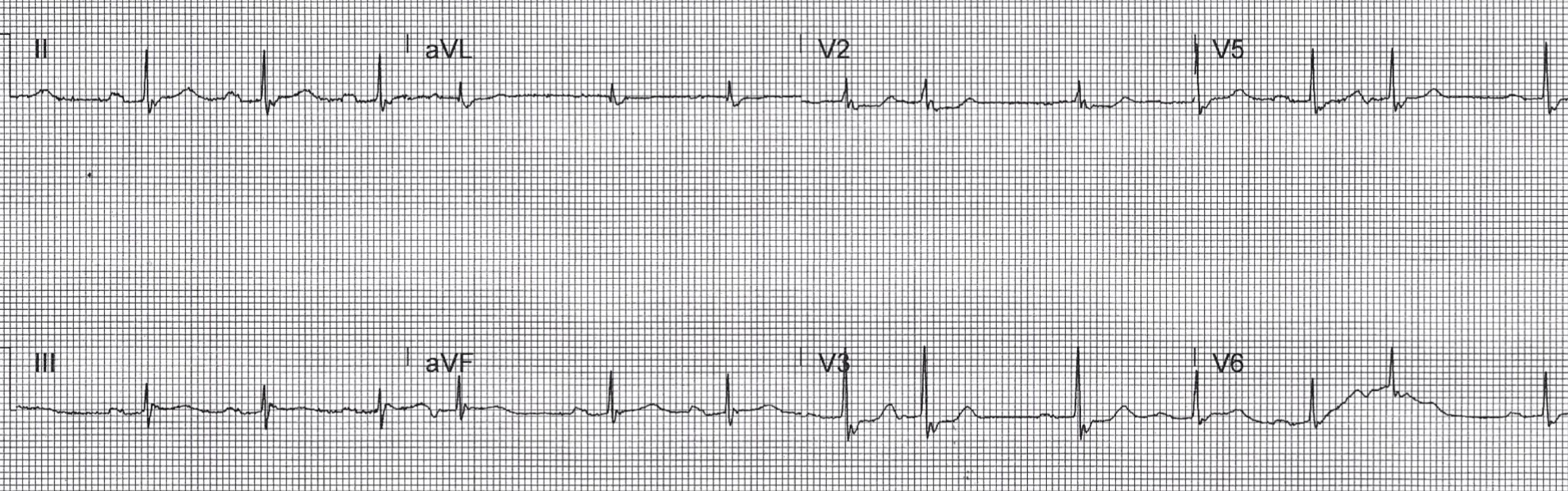
Computer read: NSR, first degree AV block, PAC, RBBB
Actual: pseudonormalized T-waves = reocclusion inferior wall, and ST depression in V2/V3 concerning again signifying posterior MI
CASE CONCLUSION:
Cardiology paged with initial ECG with concern for STEMI and then with each subsequent ECG and each troponin (levels were 40, 250, 2400) but would not take patient emergently to cath lab despite that plus a BP in the 90’s and refractory chest pain. Next morning cath showed a 100% RCA occlusion. Peak troponin was “>5,000”. EF was 35% in the cath lab with hope that it would improve from recovery of stunned myocardium.
